Dr. Herbert Schilder used the title, "Predictably Successful Endodontics," to describe many of the lectures he gave over about a 40-year timeline. In the most simple and direct way, these words promise longterm treatment success that is not only possible, but attainable...
"The Look" & Disinfection Is "The Look" Controversial & Ingle Symposium Inspired Q&A
The show begins with Ruddle & Lisette discussing an unusual service that you might want to consider adding to your practice: Vampire fangs! Then, decades ago, Herb Schilder described cases that fulfilled the 5 mechanical objectives as having “the Look”; is this controversial? After, Ruddle and Lisette do a Q&A with disinfection-related questions from lecture attendees at the USC Ingle Symposium earlier this year. The episode concludes with a couple case reports; can a case be successful and NOT have “the Look”, or vice versa?
Show Content & Timecodes
00:16 - INTRO: Vampire Teeth 08:34 - SEGMENT 1: “The Look” – A Controversy? 34:49 - SEGMENT 2: Disinfection Q&A – Questions from the USC Ingle Symposium Attendees 55:03 - CLOSE: Case Report – “The Look”Extra content referenced within show:
Other ‘Ruddle Show’ episodes/podcasts referenced within show:
Extra movie/video content:
Downloadable PDFs & Related Materials
It is globally accepted that 3D cleaning and disinfection are central to endodontic success and that bacteria are ubiquitous in endodontically failing teeth. Yet, there is ongoing controversy regarding the very clinical methods used that directly influence eliminating these microbial invaders. The role of bacteria in the pathogenesis of endodontic disease is well established, and therefore, it is critical to eradicate these pathogens by employing the highest level of presently developed standards.
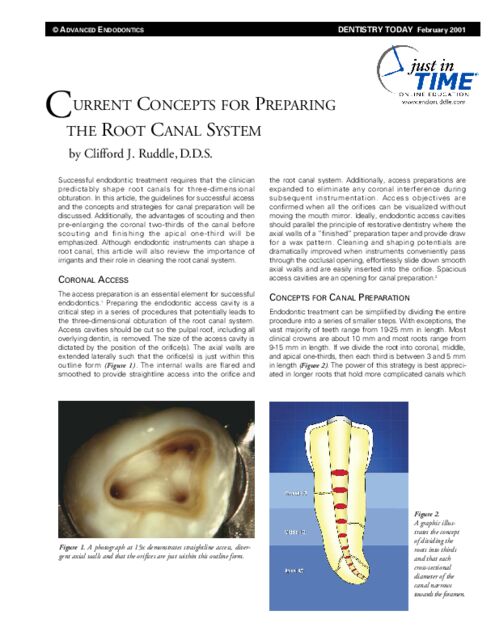
Successful endodontic treatment requires that the clinician predictably shape root canals for three-dimensional obturation. In this article, the guidelines for successful access and the concepts and strategies for canal preparation will be discussed...
This transcript is made available by The Ruddle Show in an effort to share opinions and information, and as an added service. Since all show text has been transcribed by a third party, grammatical errors and/or misspellings may occur. As such, we encourage you to listen/watch the show whenever possible and use the transcript for your own general, personal information. Any reproduction of show content (visual, audio or written) is strictly forbidden.
INTRO: Vampire Teeth
Welcome to The Ruddle Show. I’m Lisette and this is my dad, Cliff Ruddle.
How you doing?
Pretty good. We’re on Show #95, so I’m excited about that on our road to 100; we’re getting there.
Yeah, and you know thanks from the audience out there. You’re signing up to RUDDLE+ and we’re pretty excited about being together to go forward.
Okay. Well you might be wondering about this graphic behind us. Every now and then we like to venture away from the concept of a traditional dental practice and give you some ideas of how to use your dental skills in creative and unique ways. On the show we’ve talked about the sought after position of a hockey team dentist. We’re talked about the possibility of getting involved in forensic dentistry for those of you who are interested in solving mysteries. Well what about supplying dental fangs to all of your patients who have a morbid fascination with vampire cultures?
I’m only half joking, because this is actually really a thing. Maybe not so much in rural areas, but in big cities there are so-called vampires. So what exactly are dental fangs?
Well dental fangs are custom restoratives that go over existing, healthy teeth, and they can come on and off as necessary. So you can have that spontaneous vampire look, if you so desire. And all the materials are usually composite, resin or porcelain even.
Sometimes I saw even gold.
Yeah, thank you! Some of them, I guess to get a little different effect, they have gold, solid gold. And so they’re removeable, and that’s the good part because you can do this temporary transformation.
Okay. When we were searching for information on this topic, we got a couple different perspectives. On one website, Vampires.com, they noted that it might – your Christian dentist might not want to give you, the vampire patient, fangs. They said though that if you can’t find a dentist, you could easily shorten your front teeth and have your canines filed.
In other words, a very invasive procedure.
That doesn’t sound ideal. If you can find a dentist, they suggested the tooth cap option that you mentioned. And we actually did find a Southern California dentist who offered this service on their website. On the website they talked about the benefits of having fangs, who are the ideal candidates, then they went into the whole installation process; which is what?
Well I think we need to really stress the consultation. Because the consultation is where you’re going to express everything you expect from these vampire teeth, and of course the professional is going to tell – I’m assuming the patient – is going to tell them the risk and the pros and cons and different things like that. So you need to really be aware of what’s involved. If it’s a go, and they say let’s go, if you have oral scanners. that’s probably the simplest because you just scan the tooth and electronically you can go to a lab and they can download the measurements, and CAD/CAM can start to mill it.
So I guess the other thing is though, I was thinking more like what I went through back in the day. I was thinking there’s impressions and you go to the lab and pour up a stone die, and you sent it off with instructions to the lab, and the lab might have a few questions because they don’t make vampire teeth routinely, so they might want to know what the Hell is going on.
But anyway, you need that consultation and hear all the patient’s expectations. Discuss price, how many visits, etc., etc. If you think there’s things that you think could go wrong, you’ve got to explain that. Like it can inadvertently pop off, you might swallow it, you might do this. But those are consultation things.
All right. Well what – are there any prerequisites or requirements?
Well what you showed me in that article that was from a dental practice that does this in Southern California, is that before any fangs are made – no, no, no, no fangs, there’s the journey towards oral health. So it starts with a full mouth examination, models, x-rays, the whole thing that you do if you’re matriculating a new patient. And if there’s any caries, those will have to be cleaned up; and that would be good, right, we’re all saying fine. Crowns might need to be placed if teeth are badly broken down. Everything has to be healthy periodontally as well, and the occlusion has to be somewhat good. And when all that is done and everything is cleaned up and they’ve declared oral health lives and exists inside your mouth, you get to have fangs.
Well this is actually one of the reasons we’re doing this segment now instead of October right before Halloween, because it sounds like this is actually quite a process. And sometimes dentists’ offices are booked a couple of months in advance, so you might want to get started on this now if you want to have vampire fangs for Halloween.
So you mentioned – I’m now going to the drawbacks – you mentioned one might pop off and you swallow it. Is there anything else you should worry about?
It would all come to the fitting, because if they fit right, I would like to think your patients can close their teeth with the fangs installed. So if they can’t, then there’s going to be prematuraties when you occlude; and you don’t want to pop this thing off because then you could swallow it or aspirate it. Ooh, an aspirated fang is quite bad!
But I loved the part – I thought the guy really was superseding fangs and he was a businessman. Because he got all this dentistry to come in through this advertisement. So like great marketer, genius ploy. And then you get them all healthy and you get all your dentistry done, your production is good, the patient is paying wildly, they think it’s terrific. Because at the end boom, bang, bam, you get fangs!
Yeah. You did mention to me before we started the show and I thought it was kind of funny that you said that you should try to avoid any romantic endeavors because you could injure the other person.
Yeah, I’m thinking you’ll probably be careful that you don’t bite down and that thing could hit the lower arch and cause injuries. Yeah, be careful with your romantic maneuvers.
Okay, well I guess maybe it’s worth it if you really want that look. So if you’re looking – if you’re a dentist looking to expand your practice, maybe you happen to have an interest in vampire and gothic culture, and of course you’re not a Christian, then maybe this is a service that you want to provide in your office. So something to think about.
Okay, well we have a great show today. We’re going to talk in our next segment about a different kind of look; Schilder’s look. So let’s get to that; that will be exciting.
SEGMENT 1: “The Look” – A Controversy?
All right. So when clinicians share radiographs and digital images, you have probably heard it said that certain cases have “The Look.” So in modern endodontics, “The Look” refers to Herb Schilder’s Five Mechanical Objectives for predictably successful endodontics. Fifty years ago Schilder defined the five mechanical objectives for shaping canals that would facilitate the cleaning and filling of root canal systems, while simultaneously fulfilling the biological objectives. And this has long been the standard in endodontics, and it’s an important part of Schilder’s legacy. There’s that word again, and we’ll get back to that a little bit later.
Now in recent years, there’s been a group that has emerged that has maintained that the concept of “The Look” is outdated. So we are going to – today we’re going to revisit the five mechanical objectives, assess if they are still relevant, and then discuss why some people might find the concept of “The Look” problematic.
So to start, why don’t you just get going with the five mechanical objectives.
Okay, I can just do this over here. And what I’ll tell you is that these objectives came from Dental Clinics North America, 1974 – April edition. So for me, this was always my bible – did you hear 1974 – that’s the year I got out.
So the five mechanical objectives. I want you to look at the graphic on the right, and it’s an untreated molar, obviously. But I want you to look on the left, and we have a funnel-shaped form, we have a continuously tapering preparation, maintain the position of the anatomy, maintain the position of the foramen, and keep the foramen as small as practical. So that I read back to you. But now we’ll go through each five of those, and I’ll have another word or two. But the point is we’ve talked about this several times over several years on various occasions. So we’ve always talked about this, because this is what should be the guiding light.
So what I want to say on this one is, a funnel can be flexible if it’s the right material, and you can have a funnel with different tapers and cross-sectional diameters as you go along that funnel. And if that funnel is flexible, you can bend it right over and superimpose it over the canal you’re going to treat. That would be Number 1. Generally speaking, Number 1 is a continuous, flowing funnel.
Now in compliance with Number 1 is Number 2. And in compliance with Number 2, it complies with this funnel, but it goes into it a little bit more deeper where every cross-sectional diameter as you move down the canal is getting smaller and smaller and smallest towards the terminus. Said opposite, it would mean going from apex to crown, you would be getting bigger and bigger; bigger as you move away from the foramen. So these are important concepts and that’s Number 1 & 2.
If we go to Number 3, what you’ll notice is that it is maintain the original anatomy. Now in our films we see mesial to distal; that’s obvious. But we’re not seeing the curves in and out of the buccal/lingual dimensions of the film. So that one’s really talking about flowing with the canals. Herbie talked about – I shouldn’t be irreverent. It’s Herbie to me, but Dr. Schilder to you. Anyway, he really wanted to talk about canals flow within the roots that hold them. And there shouldn’t be steps and irregularities; they should just be moving like a nice, smooth flowing river – flow. And that’s maintaining the original anatomy, and in multiple planes. And remember; we’re talking about three planes, and we’re talking about three planes in any given level of the root. And then you have another three planes, and the canal comes – so multiple three planes, and then different planes.
Okay, what was our next one? Four. It was maintain the position of the foramen. One of the most common things I saw in failures was people would relocate the foramen on the external root surface. So the foramen physiologically in its relationship to the bone should not deviate. They should always maintain the orientation. It might get a little bit bigger, but we really don’t have to do a lot of work enlarging the foramen if we have all of the other four I just talked about.
And finally I guess the last one would just be keep the foramen as small as practical. Now when I say practical, a lot of times kids come in. They have big canals, big systems, and you’re first file to even snug in apically might be a 50 or a 60. But Schilder did say that in general, for the vast majority of cases in molars, it can be he said the size of a #3 file, which the group out there has never heard of. But it would be equivalent to today’s Iso 25, size 25.
So that is the mechanical objectives, and it’s something that I used on every single case I ever treated. You might not understand this. So I hold up a post-operative film before digital. What do you think I’m saying? Oh gee, nice job Cliff! Have the staff hit me on the back – it’s fabulous! It’s like artwork; let’s close the office down. Let’s have some wine.
No, what you do is you hold the film up and you do it quietly. You go funnel-shaped form, maintain the position of the foramen, mmmm, you do a checklist. This is the checklist and it’s a checklist so when we take away the graphic that we saw earlier, now we can take these objectives. And as you look at these objectives, look at the case and ask yourself; does it exhibit this, this, this, this and this? Check; good case. Nice; next case.
If you see something that you don’t quite like, figure it out; next case. Don’t linger in the past and don’t go back and start to be a hero. Just learn and move on.
So I think this is a nice case; it’s not a hard one particularly, but it’s got a flow and “The Look.”
Well just looking at the mechanical objectives, they really seem to just be common sense and logical. I’m not really sure why anyone would argue with any of these. And even if you were a proponent of minimally invasive endodontics, I don’t think that you would have a problem with these objectives. Schilder doesn’t give any dimensions. He just says keep it -
Say that again?
He does not give any dimensions. He just says keep the foramen as small as practical. Meaning that you just need to make a big enough shape so that you can clean and obturate, whatever method you choose to use.
Bingo!
So I have a couple questions related to dimensions, and the part they play in the idea of “The Look.” So first it says continuous taper, but how important is the percentage taper of the preparation? Is that something you need to be thinking about, and what role does deep shape play?
Very good. The first thing I would ask a colleague – you just asked me. I’m a colleague of yours, so you’re a colleague of mine, so I would say this. How do you intend to disinfect? What’s your cleaning method? See, back in the day when Schilder lived, and most of my career when I lived, shaping occurred over a longer period of time because we didn’t have all the technology. So you had your irrigants inside you a lot longer than in the current days. So the first question is Doctor, in the current era, what is your disinfection method?
I would then want to say okay, great. And then what is your filling method? Because there’s a variety of different things being taught now; single cone, different sealers that emerged with no real efficacy behind them. We all want to be modern and new, so we jump on these things. But I would have to start off with if you know what your cleaning method is, and if you know what your filling method is, then I would go back and say if I have a laser now – you know, 29/40, that wavelength – if I have GentleWave, which I don’t subscribe to but it’s considered by some to be at least better than handheld irrigation; I think that’s irrefutable – but I’d want to know that. Because a lot of the people that have gone to lasers and GentleWave are making 17/03s, 20/04s. In other words, you heard me say the preps have gotten decidedly more minimally invasive, and they’re much more skinny. Those can’t be cleaned in any other way than maybe a laser or GentleWave at this time.
So I have evidence. In fact I found a tape last night; I was going to ask you if we should ever show it. It’s case #816 from Gary Carr’s lab. It was done in the field on a molar, guy did a 17/03 prep, Gary Carr clipped it, it was extracted – it failed and the patient didn’t want to fool around with retreatment. Gary did a biopsy on it, and on the apical third of a 17/03 prep and the colleague uses GentleWave, he said there were sheets and beds of tissue left behind. But we’ve known this for years from other research. So I don’t really subscribe to these skinny shapes, but that would be the first thing I’d want to know is what is your next two steps going to be, because that would decide a lot.
Now specifically – I can make a disclosure. I have team, Machtou and I won’t name all the names. West was on the ProTaper team, but then there was the WaveOne team. But WaveOne Gold and ProTaper Gold and ProTaper Ultimate, automatically, without trying to use 10-16 instruments – that’s what we used in the day – about 11 files, and add about 4 GGs to that, and you had an armamentarium of about 15 instruments. You don’t think about this much anymore, going through all those files and what are they for because you’re getting those shapes exactly on your instruments. It’s working exactly as the Schilderian philosophy. That’s why Schilder embraced ProTaper towards the end, because it absolutely slewed him.
So back to ProTaper Ultimate, and F2, 25 at the tip; at the top, 16mm away it’s 1mm. Come on people! That is a very conservative, because where you get the deep shape is apical and around curvatures; but we’re keeping the body of the canal slimmer because the maximum fluid diameter is 1mm.
So I think the last thing I’d like to say is if you get the shapes of the WaveOne Gold or ProTaper Gold, or WaveOne primary say, you are going to have a deep shape. Let me explain quickly. Deep shape means you have volume to accept more fluid. So if you have more fluid, you’re probably thinking gee; if I have more fluid, more fluid to exchange. If I can have a greater volume of fluid that’s not just sitting there and it’s activated and it can start to exchange, now I have a capture zone. When you have deep shape, it holds your solutions inside the canal. When you have shapes that are kind of parallel, especially if they’re skinny, it’s a two-way street. Stuff can go up and evacuate and vent, but stuff has an easier chance – as we saw early in the WaveOne we saw that a lot; the accidents, the bloody canals and things like that – because there was no resistance form to hold your solution. And finally, deep shape is a wonderful capture zone for warm gutta-percha.
Okay. Well another question. If I’m looking at it – and this is related to dimensions too. If I am looking at a case that has “The Look,” approximately what fraction of the root width, in your opinion, would the finished canal preparation represent?
Excellent. I was working with my multi team yesterday. It seemed like a really great day, because we were looking at the various shapes. And I want to come back and say one thing about a 25/08 F2, or a primary WaveOne. It has 19% more volume than your favorite instrument that you like to use; 25/06.
So let’s say it again... 6% holds 19% less volume of fluid – cc’s, ml’s – than an 8% taper. So changing the taper changes the volume, and changing the volume means the potential to encourage better cleaning.
So back to your question. When you look at a film, we’re always taught to look at the body of the canal. In other words, there’s the coronal one-third, the middle one-third, the apical one-third. So we divide the root into thirds. I’m not looking at the apical third for what she just asked me. We’re looking at the body of the canal, the upper two-thirds. And it seems like both natural teeth, untreated, and well-treated canals often end up at about a third to a quarter. So if you look mesial to distal, the mesial to distal dimensions, you have about – the canal would occupy about a third, or it could occupy a quarter. So somewhere in there, a quarter to a third is going to be absolutely fine. You’ll have endodontically strong teeth; you won’t have fracture potentials. What my team and I were doing yesterday, to get back to that -- we were looking at just a lot of virgin teeth, untreated, on Cliff’s pre-ops.
Many orifices – as I’ve said a thousand times – when you open the teeth, you’re the first guy in, first lady in, they’re already 1mm. So you look at a lot of films and you look at the coronal two-thirds of the canal; it’s already occupying maybe a third of the mesial to distal dimension. I think that’s fine. I think it’s absolutely fine.
Retreatment... All bets are off. Because they can be much bigger based on history. And then the age of the patient and how big is the premature, the immature root canal. Oh excuse me; root canal system.
So you get dealt a deck of cards; people come in. And just be aware of these concepts and don’t beat yourself up too much if it’s looking like – gee, a third, a third, a third. That might be ideal; you might want it to be a little smaller. Certainly the minimally invasive people are more like a quarter.
Okay. Well what about seeing filled lateral anatomy? Because if you’re looking at cases that have “The Look,” don’t you generally see maybe some filled lateral anatomy? Even though the five mechanical objectives are just about the main canal; right?
They are and they aren’t. Because Schilder was probably smarter than most of us. He realized that if you took his five mechanical objectives to heart and actually developed those kinds of shapes on a go forward basis; he knew you would get the root canal system clean, because that was the whole reason for his chapter. It wasn’t how to clean canals. The name of the chapter is “Cleaning Root Canal Systems.” So he realized if you developed those, the anatomy would come.
It’s kind of like in golf, or anything you do in a sport. You work at it, you’re floundering, you look awkward. But at some point you begin to have a breakthrough, you get a little bump on the plateau of practice and you go to a higher level. And now you stay in that plateau a little while, then you can boom, make another thing. Like you hear this show and for sure I know you’re going to sign up for RUDDLE+, because you’re going to say I want that next bump on the continuum.
So anyway, that’s kind of what I would say about that. You know, why do some of us see bifidities, trifidities, loops, fins, anastomosing, multiple portals of exit? This is the language that Schilder brought us. This is the language because we discovered it through looking at our work.
So my impressions are that not a lot of people that are doing skinny shapes are getting a plethora of lateral canals. I’ve said this before; John West has done this for decades. He’s said if I shape the mother canal, how many portals of exit do I usually get? And Johnny’s getting, I think, a little over three. So for every one shaped canal where his file goes there, he's getting another one or another one. Three portals of exit with one apical where we put the file in.
So I think that when the canals get really skinny, if you don’t have a laser – I’ll keep beating this to death – you’re just not going to get anatomy. I’ve looked at hundreds, maybe thousands of cases filled with BC Sealer, small minimally invasive preps; you rarely see any evidence of the thrill of the fill on post treatment films.
And we’ll get to that a little bit later in our discussion.
So just to close out with the mechanical objectives. They seem very logical. They also are just not overly restrictive with dimensions that need to be followed. So it seems that they allow for both minimally prepared shapes, and then also for larger, more root appropriate shapes as well.
Notice the word she used; it was very, very good. It was so Ruddle, I’m championing her. “Root appropriate.” Because a lot of this misinformation comes from oh, it’s too big. Too big relative to what? So is it root appropriate should be the way we language that; thanks.
Okay, we can say minimally prepared and then root appropriate.
There you go. Let’s get our communications.
So if it allows for both minimally prepared shapes as well as root appropriate, larger root appropriate, prepared shapes, why would the concept of “The Look” cause any controversy?
Really? Actually, to be honest, I have no idea. If you use one’s mind, critical thinking, curiosity, imagination. I have wrestled with this ever since this new wave came in about 10 years ago. I know who the group is, you know who the groups are. They’re in every country and they’re a little band, and they’re almost fanatical about “The Look.” And they compare “The Look” to overzealous shapes that are not root appropriate, and they look at some endodontists that do it, and they blame that as that’s what Schilder taught. Schilder never taught that. She said three times; it’s a dimensionalist concept. And she mentioned specifically; the foramen is dimensionalist. The whole length of the prepped and developed shape is basically subjective, and you can do many different things as long as you stay – she said the range – between minimally invasive and root appropriate.
So I think – I don’t know. I looked at you weird just a while ago, because do we live in a cancel culture? Have you ever heard of that?
We do to a large extent.
We have an endo. This would be Exhibit A. Just cancelling the book. Cancelling “The Look” because it doesn’t fit your ideas. And then you make fun of it, and then you try to destruct the idea and destroy people, and that’s what you get. But “The Look” is very much alive. Schilder used to say: things that look right are right; things that don’t look right aren’t right.
Okay, well maybe some of this controversy is coming from what you just mentioned a little bit earlier. It does seem that seeing filled lateral anatomy is an important part of “The Look.” And I can understand with the warm vertical technique how you’re pushing – hydraulically pushing gutta-percha – that you would see the lateral anatomy filled.
But I’m just wondering if clinicians that use a single cone and BC Sealer can see a lot of filled lateral anatomy. Because my intuition would tell me no, unless the flow properties of the BC Sealer are so superb that it just effortlessly flows into the lateral anatomy.
That can happen. And I won’t mention names, but on the AAE Discussion Forum, there’s a handful – this is worldwide – of laser users. And I will say, I will happily admit, that their preparations are very, very small by my standards. They would not be possible to be cleaned, except for that kind of high-end technology. And they do show lateral anatomy. And you can kind of see that I can get a pulse on the group. Some people are going well that’s nice; I never saw that. Well then they tend to trivialize it. It doesn’t matter. Do lateral canals matter? And they start going into all these different assertions to trivialize one’s work.
I do not – I’ve seen some GentleWave lateral anatomy, but it’s usually with clinicians that are shaping pretty much Schilder driven. Like Cami Ferris; she’ll be a guest coming up. She’s Schilder trained. She shapes to about a 25/08, somewhere in there. She’s tried to reduce her bodywork, but her deep shape is just like what we’ve talked about. She shows anatomy routinely.
So we want to teach things that the masses can do. We want to teach things that every clinician can do if they so choose. And it shouldn’t be so technically challenging or so costly that they’re out of the game.
And just to remind everyone. We did already mention several times in our show that general practitioners do about 80% of the endodontics in the States.
So why do we care if they do root appropriate shapes, irrigate like we’ve been talking about? And you know what? They send us cases. For years and years when – she used to work out of the office; now we work together here on the set – but she used to see the emails that came in. And all the people that took our course, they’d show their first furcal canal, their first lateral canal, their first apical division, bifidity. And they were thrilled.
So that means it’s transferable; anybody can do it; it’s a choice.
Well I think another argument that people who have a problem with “The Look,” an argument that they present is that sometimes cases fail and they have The Look. And then other times cases are successful but don’t have The Look at all. So probably these cases represent more of the exception though than the rule.
Yeah. I mean we all have – we can feed our egos or our argument with an anecdotal, sometimes event. In other words look, I got a lateral canal; and my shape was like a 10/02. A round of applause. But is that reproducible over and over across decades of practicing on patients you’re supposed to be serving?
So yeah. Schilder – I’ll repeat it – he said things that don’t look right aren’t right. So I think it’s fine to say do you get the anatomies routinely? No. John West, Machtou, Castellucci, Cliff Ruddle, and I could just keep going because I don’t want to embarrass myself and leave you off the list. We taught root appropriate shapes; people were routinely filling anatomy. On the AAE discussion forum, the people that do routine cleaning and shaping are not showing anatomy because their shapes are too small.
Well I know there’s an expression, you can’t judge a book by its cover. But you probably can tell a lot about a book by its cover, and why not appreciate the beauty of the cover if it’s beautiful? I don’t know. I think the mechanical objectives are a big part of Schilder’s legacy – there’s that word again. And whether or not Schilder realized it, I think part of the genius of his mechanical objectives are that they appeal to logic and common sense. And the fact that he doesn’t give any dimensions kind of gives them more of a timeless nature. Because if you would have stayed in certain dimensions, all of a sudden they would have become a lot more transient and maybe not held the test of time.
So I think that is an important part of legacy; to have a certain timelessness about your work. I think the most powerful legacies are those that transcend time and they endure.
Oh, you mean like e=mc2?
Right. Well later on in the show, when we close the show, you’re going to show some cases related to this idea of “The Look,” right?
Yeah. At the wrap up, we’re going to take the four examples: 1) looks bad, is bad; 2) looks bad, is good; 3) looks good, is bad; 4) looks good, is good.
Okay, well can’t wait for that. We’ll see that soon. Thank you for the information.
SEGMENT 2: Disinfection Q&A – Questions from the USC Ingle Symposium Attendees
Okay, so at the end of last year, you gave a lecture at USC for the John Ingle Symposium – that’s at the annual meeting – and your lecture was on 3-D disinfection. And we actually have that lecture available to watch on The Ruddle Show website as a special report. So you might want to see the lecture if you haven’t already.
Now at the end of your lecture, which you submitted a lecture, at the end of your lecture you did a live Q&A with – it was an international audience, I believe.
Right.
So Ilan Rotstein – that’s his name, right – he asked you questions and you answered.
Professor Ilan Rotstein, greetings. I know you’re watching and so thank you for that opportunity.
So we’re actually going to re-do this Q&A with the questions that were asked him. And you can go – well I guess you won’t have access to the live Q&A that he did, but hopefully the answers will be similar to what they were originally.
All right, so are you ready for the questions?
Well to say that my answers – there’s a 36-minute Q&A and my Q&A is going to be – you tell me – 10 minutes? So we’re going to do a -
Can it be shorter?
We’ll do a summary.
Okay. But we’re going to still ask all the questions. So the first question is this. What is the ideal size of EndoActivator tip to use in molars? What tip do you recommend?
Okay. Well we talked about this even earlier in the show today. We talked about – Schilder always advocated about a 25/08, or 10 if that helps. So ProTaper Gold, ProTaper Ultimate have 25/08, and WaveOne Gold, its primary, the primary one specifically, is a 25/07. So we have seen in the literature – since these files were launched decades ago, we have seen much of the literature showing disinfection in these kinds of shapes.
So these are the kinds of shape that have been advocated for decades, that when developed and carefully executed, will let you choose your tip. And typically if you’re shaping somewhere in this range, you would be using the EndoActivator, specifically the SmartLite Pro EndoActivator, and it would be the red tip. And the red tip is +/- a 25/04. Now I say +/-; these aren’t machined or polymers so they don’t cut; they’re intentionally non-cutting. So the ejection molding +/- a 23 or a 27, is in the range of tolerance. The point is, choose the tip that fits within 2mm – just write it down – 2mm of working length; that’s one. And the second one is loose.
So if the tip is tight, you need to either develop a little more shape – not more than this, but you might be using like an 04 or an 06 – so you might develop a little bit more shape if you were so inclined. Or you could go to a smaller tip, and we also have – this is red; we also have a yellow tip.
Yeah, but would you still get the result if you put a yellow into this size canal; because you would just get more agitation maybe?
Um-hmm. Yeah, so -
Still using the red?
Well we have a blue one, because sometimes kits come into the office. Remember that case I was just showing you where it was a third/third/third on a virgin tooth? Well that’s a big one, but there’s a lot of them that come in and they’re really skinny. Like older people like me and they’re calcified and more mineralized. So you might not want to just open it up to fit the tip, but you could go to a smaller tip where you’d have that 2-Alpha. Remember, we don’t want the tip to be frozen. The whole principle is it must slap those walls and fracture liquids, and to do that, it must move.
Okay. Next question. How do you establish working length? What is your method?
Oh this is really easy. It used to be via radiograph was our go-to, right? Just take an image, take a working film. But then apex, electronic apex locators came on the market. They became very reliable, even back in the day when I was younger. So now it’s the – well I guess we can go one more. It’s either an electronic apex locator, and my second opinion would be radiographic image.
And one thing I talked about – so this is your first go-to right here. Then if you want to sometimes get corroborating information, do both. And then a third idea that I can put down here would just be paper point drying method, and I’ll explain that.
If you put a paper point a little bit through the foramen, the part of the paper point that’s long is usually red. That part of the paper point that is clean, white and dry, is the measurement from here up to your reference point. So you might have this thing come up like this, and this would be your measuring point; if you had a rubber stop, you’d put it on that. And you’d be measuring it from here, up around to there.
So this is, unfortunately, only possible once you’re done. So this isn’t going to help you find working length on your 10 file, because it won’t fit in there. But when you’re all done, where do you pack to? That’s the most common – Ruddle, where do you pack to? Is it a half millimeter short? Is it flush? It’s depending on the paper point, because this out-performs these two at this level. If it’s red, it’s beyond. So you just measure the dry part, cut your cone back and there you go.
Okay, next question. With the advancement in biomaterials, many people are injecting sealers, leading to overfills. How do you apply your sealer and do you subscribe to injecting these bioceramics into the root canal?
Well this question – it came in from somewhere; I don’t know what country or what colleague – but I had much more to say about this on the actual, live Q&A.
Well I remember when I was watching it; your reaction after this question was asked was wow! I remember you said that.
Well okay. So it’s a fair question though. It’s just that I don’t use BC Sealer, so I don’t subscribe to that. That’s another story.
Well I better say a few words. Because so many of you jumped in the pool, and on the way down you’re thinking my God, there’s no water in this pool. So you’re off the high dive – I hope you were so you get a maximum impact. Anyway, I don’t use something that isn’t necessarily reliable. Do we know for sure? Is the literature in? Is it completely defined that this is the new future and the way to go?
But when I had Josette on the phone – Camilleri, Dr. Camilleri from the UK, Birmingham. When we had her on the show, she didn’t have a problem with it, except she says it’s really a problem if you mix it with – she calls it synchronization. But if you’re using sodium hypochlorite, 17% EDTA, and you’re using BC Sealers, that’s a problem. And she said you’d better be thinking about using a buffered saline solution. You’d better remove those remnants of sodium hypochlorite and EDTA, because they will alter the working physical properties of the BC Sealer.
So the reason – I don’t want to go into that now; that’s not her question. But I don’t want to just be flippant and say I don’t use it because it sucks. I want to tell you why I don’t use it. I’m using a 50-year-old sealer. It’s had hundreds if not thousands of papers showing its efficacy and it’s working. And so I don’t just – like Bucannon. I mean Steve just announced a few years ago: after 40 years of using curved pulp canal sealer, I now want that biocompatibility, and I’m jumping sealers. Well that’s crazy. Nobody jumps sealers unless you’re getting paid.
Especially if you had a good experience for 40 years.
Oh, did this stand for bull****, or was that for Beaufort Stanley?
Does curved pulp canal sealer have regenerative characteristics?
It does, but not in the way the audience thinks. See, the audience gets caught up with biocompatibility. Well what about splashes of curved pulp canal sealer? The bone is completely grown in around the root – I guess we should make this a little bit visual.
So you did a root canal and you picked up some very nice anatomy along the way. And you’ve got this big lesion and you’ve got buttons of sealer and you’re all filled and you’re full. Can we call it regenerated if I see this bone all grow back? And do we care what that puff is? Is that a BC puff, is that a curve puff, is that another kind of sealer puff, is it a Resilon puff? I mean if the bone’s working, it’s a regenerating material. I’ve always said endodontics is a regenerating material. Because properly performed, it’s a cornerstone of starting a reconstructive dentistry.
Okay, this next question is probably a quick one. What is your opinion about the EndoVac for cleaning root canals?
Never used the EndoVac. John Schoeffel made the EndoVac; it got a lot of noise. And in fairness to John, up until that time, more or less, we had been doing handheld irrigation. So it was the first way – the first thing that came along where you had a canal, and let’s just say it looks like this. In this zone, you had to prepare your canals to > or = 30, just to get the cannula; just to get the cannula in there. So the cannula is supposed to go down to within I think about 1mm of length. Well I never use anything where I have to make the canal fit my method. Like when I go to get shoes, I usually just get shoes that fit my feet versus them carving my foot down so I can get that shoe.
I just was thinking of something related to this. Remember when we had Dr. Gary Glassman do start-to-finish endo on our show? Did he use the EndoVac?
He did.
Okay, because I thought I remembered us talking about that a little bit in the post-presentation discussion.
Let me say it different. It’s not wrong to use the EndoVac. But in smaller canals – which a lot of endodontists see because we get the tougher ones – I do not like to have to machine this out. I hate that word: machine. I like flowing shapes like Schilder talked about.
I don’t like to have to machine out the apical part of a canal, just so I can take a tube and stick it in here. And then it occupies all that space, and then I’m going to be pumping water. So I’m going to be vacuuming. So your assistant is irrigating over here with a syringe; it will overflow the tooth. But wait a minute. The suction – the suction, the vacuum goes through the cannula and it’s pulling in this direction. So before this can run off, it’s a loop. So you’re creating – for effect, you’re creating an irrigation that goes down the tube; but before it can go out, it’s being pulled back up. So you’re having reflux backup inside the tooth.
So it was a good idea because it was the first maybe effort to be more active; active irrigation. Then we came along with the EndoVac, or the EndoActivator, and it can go in any shape – yellow, red, blue. It’s easy to use, it’s handheld, there’s no cords, there’s no junk and lines and stuff. So simple, simple, simple.
Okay, the next question Ilan said – you don’t have to answer it if you’re nervous about legal stuff. So I’m going to give you that same option that he gave you.
He told the audience, and it took him about five minutes to talk about Ruddle’s courage and boldness to speak the truth when most won’t. And then he said what you just said; you don’t have to answer this though.
Okay. Is it possible to use GentleWave if bleeding is still present?
Well see, when you get a question like that, and we’re up here and they’re out there and that was December of last year, I don’t know what that means. But I’ll try to play with it.
So you have a root and you have some kind of a canal that makes a turn. And let’s just say for some reason, there was granulation tissue inside this periapical lesion. And it gets stirred up and all of a sudden blood’s pouring back up into the canal.
So first thing I want to know when you say is there bleeding, it bleeds; is it inside or out? Is the bleeding coming from periapical, maybe even through a significant lateral canal? Is the bleeding coming from tissue that you haven’t got out yet? Is it because there’s tissue down in here that you haven’t got out yet? Or is it coming periapical? So if it’s coming from outside, you’ve probably caused a problem because you’re using GentleWave.
Yeah, but maybe they mean there’s bleeding, so then can I use GentleWave versus? I’m using GentleWave, the bleeding starts, but should I still keep going? I don’t know.
Oh absolutely.
I don’t know what the Hell they mean; the order.
Right. So yeah. I mean you have to think as a teacher extemporaneously, because the question comes and you’ve got to try to get it into that head immediately. So you’ve got to start thinking about – he’s thinking about this – she wants to know. So you’ve got to try to answer it in convoluted ways, but you’re trying to get to the bottom of the question.
So first of all, maybe you could identify inside and out. And then the 2 – you already beat me to it – were you using GentleWave? Because this is one of the things in the early days of GentleWave users, and they’ve done their homework and they’ve adjusted and modified – the old sports terms – to make it work. And so bleeding episodes apparently are down. Not completely from what I hear. But back in the day, there was bleeding on the vast majority of cases. I said the vast majority. It was on their own website. Sonendo had a website called Doc Matters, and it was a place for me and you to do our technology and report our results for everybody to hear. You’d learn from me, I’d learn from you. So if it was not from GentleWave, you’re probably in good shape.
But if you’re in GentleWave and it’s bleeding, you’ve got to control the blood. So get the platform off the tooth if you’re using GentleWave. And I would really be careful using ferric sulphates, or these vasoconstrictors, because you’re going to end up with a coagulant. So you’ll stop the bleeding. I’ve seen people take their paper point, put it in ferric sulphate, haul it in, take it to length, pump it up and down – pump, pump, pump – and all of a sudden the bleeding starts to diminish. But we used it in surgery for decades – still do – it’s one of the great hemostatics. That was black coagulum, and if you didn’t sit there with your curette and scrape that all out and promote new bleeding, then that coagulum is a culture for bacteria.
Probably if you had bleeding that was persisting, then you’d probably want to try to stop the bleeding before you proceeded with anything.
That’s what I’m trying to say. So you might use some calcium hydroxide. If you did have bleeding down here, you’re probably thinking calcium hydroxide. Calcium hydroxide. And you might have to reappoint. So that costs a visit and that’s pretty expensive in today’s world of disposables and chit-chat and wasted time when you’re not doing productive work.
So I don’t want to go off on this, because we don’t know exactly. The bleeding – let’s just assume it wasn’t from anything other than tissue left inside. You’ve got to go back and do more cleaning. If you think it’s coming from out here, you’ve probably – you could have – your files could have been long. What if your file was sticking out here, and granulation tissue, you just look at it and it starts to bleed. It's the first tissue in disease and it’s the first tissue in healing. It’s kind of like a chameleon. But as soon as you get the biology right, it helps promote healing.
So files can cause bleeding; residual tissue left behind can cause bleeding. Sometimes the canal goes around like this, but the colleague ends up over here. And if you look at this root at the end, you have the world’s biggest rip. So that would be your foramen, it used to be right there; but now you’ve moved it over here and dragged it, and so now you have this canal that’s like this, you’ve mutilated the root, and of course those are called bleeders; they bleed a lot.
All right. Well we have one more question, and we’re tight on time, so I’m only going to give you the opportunity to say a couple of sentences on it. I want to tell our audience that we recently did a podcast where you gave a very thorough opinion on this. So you might want to check out the podcast for a very detailed response. But for a short – you’re just going to give a short answer now.
Um-hmm.
What do you think about the single cone technique?
Bull****!
Okay. I want you to -
Well there’s a lot more to be said, but that’s – you know why.
So then I invite you all to go watch the podcast, because we say a lot about it.
If you want to see, Hess’ Anatomy – I didn’t say this earlier in the show.
If you want “The Look.”
If you want “The Look,” go look at Hess’. It’s a book of 10,000 sections. I have the only one in North America. As you turn the pages, you’re just stunned by how the anatomy looks. And Schilder said how could you practice a whole career and you saw any of that – ever! That means you’re missing a lot.
So you’re not going to get it with a single cone. You’ll get paid; insurance will pay you.
All right, well thank you for that Q&A. And now let’s close the show with some more cases about “The Look.”
Okay, thank you.
CLOSE: Case Report – “The Look”
Okay, so we mentioned at the close of our segment on “The Look” that at the end of the show you were going to show some cases related to “The Look.” And I think you said you were going to show 1) looks bad, is bad; 2) looks bad, is good; 3) looks good, is bad; and 4) looks good, is good. Is that correct?
Wow, yes. That always confuses me.
Well I’m going to step aside and let you show them.
Okay. So I’m just going to end this whole thing as we’re questioning; it’s a question. Is it a controversy? The Look: Is it a Controversy?
Very quick – you saw these earlier in the show. But if you start holding these up to funnel shaped form, continuous taper, maintain the original anatomy, maintain the position of the foramina, keep the foramina as small as possible; you can begin to see – that’s your post-treatment checklist. And that’s what I would say for every one of these.
You’ll also notice, because one of the questions Lisette asked me was well do you see anatomy? Well you see a lot of anatomy in cases that you’ve actually prepared well. Now we’ve talked about the third: the third, the third, the third; you can see how that kind of works. I would say we’re actually smaller if you’re going from this wall in. This is probably about a third and this is about a third, but actually very conservative for me. This is a fluted root, so this looks appropriate. And then right here – you might have missed this one. There used to be a lesion here if I showed you the whole case and all the images. You would have seen the preoperative, loss of bone, there was a periodontal defect. And I was thrilled about this. I didn’t even put a file in the middle one; that’s why it has reversed apical architecture. So even a monkey can full out of a tree, and sometimes the monkey is Ruddle. And then I saw that, and then we have recalls with the bone growing back in. The bone is depositing, it’s a regenerating procedure, endodontics must have “The Look.”
So let’s look at left real quick. We can go very, very fast and we’ll get the first one in here. So this is stuff you see every day in your practice. Whether you’re an endodontist with a lot of retreatments; you’re a general dentist and new patients move in, or maybe you have a couple here and there; and things that don’t look right aren’t right. Remember we said that. This is filled short. This is a little short, but in a three-dimensional model, that could have been the actual foramen. But what about this distance from here to here; from here to here? They’re not even. So what that means is there should be another system in here.
So things that don’t look right to Ruddle aren’t right, and they don’t hold up over time; even if you get lucky for a few years.
Now this looks pretty bad to me. But you know what? Ask a question. If you must speak, ask a question. When was your work done? About 35 years ago, Doctor. I hope my work lasts 35 years! But look; this is a really stupid little preparation here. You’ve got a silver point in the lingual. In the buccal you’re over here, but again if we look at the rules of symmetry, we’re not centered. And when I retreated this, in fact I got that and I got that.
So this one. The post is a little large; I’d like these nicked down a little bit, take that shoulder off. But kind of incomplete endodontics, spotty endodontics. But the bone; it has intact PDLs. Intact PDLs. So it’s looking good, and it’s working… It’s not looking good.
And then we do this one, and we’ve seen this a million times haven’t we? Where you trained will tell me a lot about who you are and how you approach your work. But training oftentimes was work short.
Now I understand you have apex locators; maybe you didn’t have them back then. I understand you’ve got CBCT, you’ve got all these different things and tools. But in this case, 1mm short made a difference. I had to retreat this case. It failed because of philosophy; 1mm short.
So looks good, is bad. A lot of people would say it looks good because my school taught me to work 1mm short. That has a nice, dense taper; nice, uniform taper. Oh wow, it’s bigger than the – look at this! It’s really like – a lot of you minimally invasive, you’re loving that. It’s not a third/third/third which would be towards the maximum. This is like a quarter. So it’s very nice in so many respects; just didn’t work.
And finally looks good, is good. So you can see two systems, pretty broad root out here. I’m pretty close, I’m getting glare of the screen, but I see PDL coming down like that – there we go. So if you start to look at these distances, again to just bring that back home. It has nice flow, look at apically – there’s that little abrupt rrrp (sound), recurvature back to the mesial. And good solid bone around the puff.
So real quick, just some cases that I would say developed “The Look.” Did you notice something today everybody? All the audience around here. Did you notice that we’re showing only maxillary bicuspids? I would have loved to do this. We started to do this and we were going to show a little random of all the teeth in the mouth; and it got too confusing because there were hundreds of teeth to choose from. So we said let’s just take maxillary bicuspids as an example, and show a few looks.
So this is carrying a bridge. It’s a strategic tooth in every sense. Two systems. Apically I see one, two, three – I see four apical portals of exit. So I think to me that has “The Look.” And I didn’t even mention, but a very, very tough access. Here’s the crown coming in like this. You can’t tell what’s under here, how it was prepared, you don’t know. So we started in right in the middle of the crown. And then as I get up here, I have to make an adjustment and come back. So really a roller coaster; kind of a complicated little case.
Another one. I want to show some strategic teeth today; teeth that are carrying large spans. And they are very, very critical for this patient. So look at this. We have a significant branch here. If you would have seen the pre-op, there’s a big black area in here and it didn’t probe. So knew it was a lesion of endodontic origin, so for me it’s fun. And sure enough, that would explain it; this is a recall. Got an apical bifidity in the buccal, and we got that little rrp – recurvature of the lingual, and then it’s bifid on top of it. So that right there is that right there.
So learn to build the Schilderian objectives into your cases. The modern-day files a lot of times will build that in for you; you don’t have to think about such a long sequence of instruments.
Different kind of a case; three systems. That has “The Look;” that looks good to me.
And finally our last collage of images isn’t showing you the whole look on anything except the middle tooth. And again, I’m very excited when I see cases like this. Again, I just keep beating this to death. We keep hearing over and over around the world; God, those big Schilderean shapes! Oh, the shaping party is over. Schilder is obsolete! The people that are telling you that are just people that are woke, and they have their own religion in endodontics and they’re quoting their own game.
So notice. If you want to go around more than 90°, get three portals of exit; there’s “The Look” and every one of these cases has significant anatomy. That was one of Lisette’s questions was, was it just the shape that he was talking about or did “The Look” mean everything? And I’m going to say it means everything.
So bring it home.
Well thank you for presenting that information. I just want to ask you. So when you fill a case and you see something like this here – I’ll circle it.
Yup.
How does it make you feel?
Oh my! How does it make? I loved endodontics; it was like a drug. It brought me back. I mean anybody that gets lateral canals, even after 30, 40, 50 years; you can’t get too many lateral canals. You can’t get tired of winning.
Okay. Well thank you, and that was a fun show. We’ll see you next time on The Ruddle Show.