There has been massive growth in endodontic treatment in recent years. This increase in clinical activity can be attributable to better-trained dentists and specialists alike. Necessary for this unfolding story is the general public's growing selection for root canal treatment...
Specific Scenario & Transportations Endo with Recurrent Caries & Transport Types 1-2-3
The show begins with Ruddle & Lisette revealing how they spend their free time on their phone. Hint: Ruddle is NOT a gamer. Then, discussions get underway about a Specific Scenario; what should you be thinking when you encounter an endodontically treated tooth with recurrent caries? After, Ruddle is at the Board taking on transportations… Types 1, 2 AND 3. The episode concludes with another Featured Grandchild segment; this time, Noah Ostovany talks tennis, training, and overall fitness.
Show Content & Timecodes
00:16 - INTRO: Free Time on Your Phone 08:12 - SEGMENT 1: Specific Scenario – Endodontically Treated Tooth with Recurrent Caries 35:04 - SEGMENT 2: Transport Types 1-2-3 1:01:21 - CLOSE: Grandkids – Noah’s Tennis & FitnessExtra content referenced within show:
Other ‘Ruddle Show’ episodes/podcasts referenced within show:
Downloadable PDFs & Related Materials
In a previous interview, Endodontic Therapy and Dr. Cliff Ruddle discuss nonsurgical retreatment and the integration of traditional and modern techniques for achieving excellence and producing predictable outcomes...
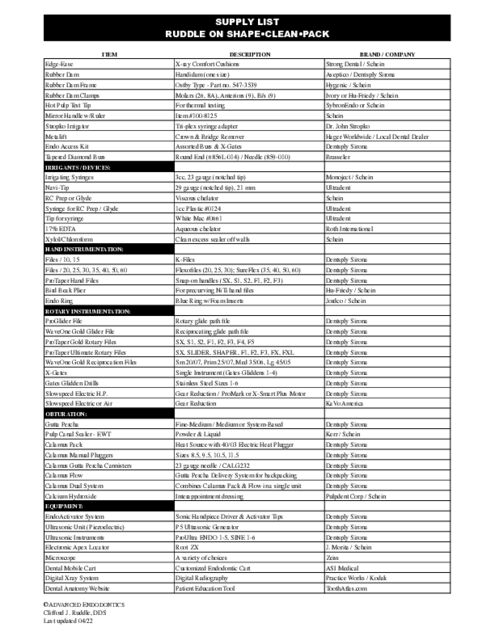
Ruddle on Shape•Clean•Pack Supply List and Supplier Contact Information Listing
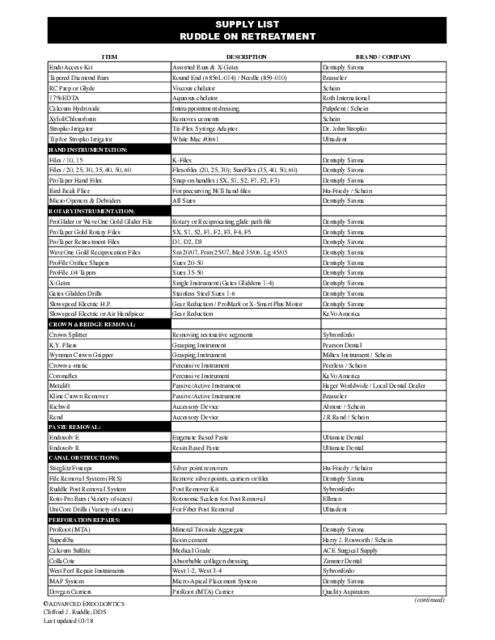
Ruddle on Retreatment Supply List and Supplier Contact Information Listing
This transcript is made available by The Ruddle Show in an effort to share opinions and information, and as an added service. Since all show text has been transcribed by a third party, grammatical errors and/or misspellings may occur. As such, we encourage you to listen/watch the show whenever possible and use the transcript for your own general, personal information. Any reproduction of show content (visual, audio or written) is strictly forbidden.
INTRO: Free Time on Your Phone
Welcome to The Ruddle Show. I’m Lisette and this is my dad Cliff Ruddle.
How you doing?
Good. How about you?
Excellent! I hope you love our graphics out there. I mean come on; look at this very carefully and then you’ll understand. We’re talking to you!
Okay. We’re going to start off talking about our phones. It’s pretty obvious that we all spend a lot of time on our phones, and that’s not just making phone calls. So even if you’re not on social media, your phone is probably still an integral part of your life. It could be your flashlight, your alarm clock, your camera, your map, your health monitor. And that’s not even mentioning all of the information, contacts, photos you have stored on your phone.
So probably the biggest reason though that people use their phones is for entertainment in their free time. So what do you do on your phone in your free time for fun?
Well yes. I wasn’t looking at – well okay. I like to use my phone to read news when I’m traveling or out and about. I can quickly – I like a paper. My favorite is the physical paper. But yeah, I like it to catch up on news. Sports would be the main – the reason really for the iPhone for me is actually not news. It would be sports and it would be endodontics. In fact, just getting ready for this show today – and we have a really nice topic coming up, but I won’t give it away – but I started Googling it and up came a lot of articles, friends of mine that had published the articles. You’ll speak about Danny – Oh Danny Boy – in Dublin.
So anyway, I like it for – you can Google information. It’s right there.
Yeah. I was actually trying to think if I could think of a game that you would like on your phone, and I really couldn’t think of any. I mean I know you like Yahtzee, and they do have an app for Yahtzee. But it’s just not the same as rolling the dice.
Oh, you’ve got to roll the dice because you get the hot hand, you know.
For me, for years, I did Sudoku on my phone. And I’m pretty much – I stick to one thing for years. Then after that, I went to Word Brain, and that’s just like a classic, not fancy at all word game, and I did that for years. But in the past few months, I’ve changed to Color-by-Number and I do this app called Zen Color. And they kind of promote it as you can relax and color by number. And I love doing it. I actually look forward to the time later in the day that I’ll be doing it. And when I do it, I have to – they don’t have a clock on the app, so I actually have to set the timer on my phone for like 30 minutes and then go do the game; because time just flies when I’m doing it.
Every now and then though, something will come up that it will say would you like to share on social media that you spent 4 hours and 37 minutes coloring? And I’m like of course I don’t want to share that! I don’t want people to know that. But I guess I just told everyone, so.
Well I was wondering; why is she telling our international audience? Everybody now knows; you’re outed!
I will say one thing. You showed me before we started this episode, you showed me some of your coloring. And what I saw immediately is it could fake anybody better at artistic things. You know, how you visualize things depends on lighting and distance and I don’t know all the variables. But I could see how it factors in for how light might pass through a fluid versus – anyway, you learn that. And so that means if you’re just free painting, that would be in your head.
No, I definitely think I would be a better artist now after doing the app for as much as I have. I think I would actually paint better.
Do they have those for teeth?
Maybe someday soon. Well I think you have some numbers to share about how much time we actually spend on our phone.
I didn’t want to share; it was kind of startling. Do you realize that the average person in North America is on their machine 4½ hours – it’s 4:38 or something – but over 4½ hours a day? That’s one day a week. How does it keep going? It’s 6 days a month, and it’s 70 days a year! That’s average; 70 days a year. Okay, that’s like honey, I’m going for January and February and a little bit of March and I’ll be gone.
That’s actually kind of scary to think that you spend that much of your life just staring at a screen.
Well what about physiologically all the other things we don’t know that the screen time might be doing?
Well, we are actually pretty lucky – I think we are – that we can remember a time in our lives when we didn’t have phones. My kids can’t. They’ve had phones in their lives their whole life, and I find myself saying stuff like I remember when I was a kid we used to have to look at paper maps in the car. Or when I was a kid and you fell asleep watching the ball game, you had to wait until the next morning to find out what the score was. Because you had to wait for the paper to come or for them to say it on the news. So it’s pretty – our phones add a lot to our life now -- a lot of instantaneous stuff.
Well I’m pretty sure the audience out there is on the phone to the same amounts of time that we’re talking about. And no doubt, you wouldn’t even want to know where they’re at and what they’re going while they’re on the phone.
And just if you want a hint at what we’re talking about, take a very close look at our graphic.
You know what? Three in five people, that sounds like 66% of the people, are actually using the graphic very well while they’re on the phone. Just don’t be calling me.
And the other percentage just isn’t admitting it.
Probably. And no doubt they’re watching The Ruddle Show is what I like to think. And then I didn’t realize zombies scrolling and rolling. I mean 48% of the people pick up their phone, they don’t even know why they’re using the phone, and they just start going down, news stories, they’re scrolling, scrolling; 48% do zombie scrolling.
Okay, well pretty much anyone you ask will say they spend too much time on their phone. And nobody though is saying I don’t spend enough time on my phone; I wish I spent more. Nobody’s saying that.
Except maybe on a rare tombstone… Here lies a fellow who wished he would have used his phone a little more.
I know. I wish I could have maximized my phone use.
All right, well we have Show 98 today, so we’re excited about that. Let’s get going on it.
SEGMENT 1: Specific Scenario – Endodontically Treated Tooth with Recurrent Caries
Okay, so today we wanted to discuss another specific scenario. A previously endodontically treated tooth with recurrent caries. Now this is concerning, because even a well-filled root canal system can become re-infected and leak when exposed to oral bacteria. So at what point does the clinician decide that a tooth has too much caries’ involvement and should be endodontically retreated?
Well today we’re going to discuss about some things to consider when making this determination; but also talk about some steps you can take to minimize coronal leakage. But maybe first you start by discussing coronal leakage and its causes.
Okay. Well coronal leakage has been something that’s been talked about for 90 years, a long, long time. I said 90, but maybe 60, 70, 80 years. So it’s been talked about.
But I would say probably just in the middle to late 80s, and then the first few years of the 90s, it really got on the map. And the reason it got on the map is people like Kimberly Swanson, Lisa Wilcox, what’s the other one there – Sandra Madison – Torabinejad. And then Elizabeth Saunders and Bill Saunders; Saunders and Saunders and their textbook.
So they published prolifically, especially the three ladies, about coronal leakage, and it really started to put it on the map for we as endodontists taking care of the rest of the seal. Because we’re always so interested in sealing the root canal system, but then there’s all of the coronal work above that has to protect the endodontics, or should protect the endodontics.
So the leakage was attributable in these papers. – so you’ll know, in these papers they leakage was intentional. I mean they took the temporary fillings out of the extracted teeth, they used artificial saliva which is pretty close to saliva with microbes and stuff, and they found leakage through broken temporaries; they found between appointments and multiple visits, broken temporaries. They found sometimes the final restoration was deficient -- not unusual. Sometimes the crown, the coronal tooth structure could fracture, and that could let egress of irritants in through a coronal fracture. Of course temporaries can collapse and break, especially if there’s cotton pellets underneath them. And then of course there’s recurrent caries.
All right. Well let’s just talk a little bit about how quickly a root canal system can become infected. Because when we did a segment earlier this season on cracked teeth, I think I remember reading that it takes approximately 60-90 days for bacteria to travel through the dentinal tubules and reach the pulp. Whereas if there’s a fracture, it travels much quicker along the fracture.
Now in an article we consulted for this segment, it was called The Implications of Coronal Leakage in Endodontically Treated Teeth. The author, Dr. Danny Bellamy, notes that some say the entire root canal system can become infected in as little as 20 days.
Yeah, I think a lot of that is back to the methodology. You can have kind of a broken temporary or maybe an ill-fitting crown, but maybe the cement just in a few microns is still holding up a seal. So a lot of the earlier work we quoted – I quoted 60-90 days, but it’s actually startling. It’s like you said, 20 days or something like that.
So since leakage can be so quick in exposed gutta percha – so we’re talking about no temporaries in these studies. This was just right through the pulp chamber and exposed gutta percha. Bellamy really speaks about the absolute importance of all the little steps we do below the orifice that can affect long-term success. So he wanted us to do meticulously glidepath management. He didn’t use the words glidepath management, but he wanted every canal exquisitely negotiated. Secured canals can be shaped, he wanted a nice flowing shape. He went to Boston University, he was trained by Schilder, so he was using the five mechanical steps.
He talked about only when you have shaping do you have like really good irrigation; and you have now a flow channel so you can do all the active ideas in the marketplace. And then of course he really emphasized – he did warm gutta percha, but he wanted a really nice, tight, wall-to-wall pack. And then he really emphasized a barrier that we’ll talk about later. And then he wanted recalls; because he wanted to keep following the cases to see how people were doing.
And especially if you notice a high caries index in some of these people, then you might want to step up, have more frequent recalls; but recalls appropriate to the patient’s mouth that you’re treating.
Yeah, I think he also mentioned just really to mitigate the amount of bacteria, have a rubber dam; it is a must. I think he said that.
Oh, I missed that part. I mean rubber dam – he said in his article and I agree completely. In 30 seconds you should have 95% or so of all teeth isolated and working perfectly in a completely controlled field. I say that because so many dentists say oh, it takes a long time; it’s pretty hard, it’s difficult. Nope, it’s not.
Okay. Well I want to talk a little bit about my own experience, and then maybe we can build on that. So I had a root canal about 15 years ago. And then 10 years after that I developed some caries where the crown meets the dentin. And my general dentist removed the crown, he cleaned out the caries, and I had to have a new crown put on. I didn’t have new endodontics though.
So today my tooth seems fine; it’s been years and I have no problem. And I actually make a point to just try to brush a little bit better. But what would be some factors to consider when deciding to simply remove the crown, clean out the caries and replace the crown versus endodontically retreating the tooth?
Well that was exactly probably the decisions that were made on your case you just described. And I think the most important thing is are you having any clinical symptoms.? So I would want to know – I’ll just say several things quickly. Chronicity. Okay, so when was the last time you were in to have a visit, Lisette? And let’s say we know that it was six months ago. Was there anything on the film then that showed that there was any caries or did it all look good?
So in other words, if you can say the caries happened sometime after she last blessed the office, the chronicity is not so great – six months is a long time if you’re talking about 20 days. But anyway, theoretically the caries might not have penetrated deep, even though there’s dentinal tubules, there’s no pulp to say ouch, I hurt. So number one, I think he would be asking you are you having any symptoms or are you asymptomatic?
The next thing I’d want to know is how chronic is it to the best of our guestimate? And then I’d want a film. I’d want more than one angle, and I might want CBCT because I want to know the quality of the root canal; how’s it look, did they get pretty much vertically to length, are they going with curvatures, did they seem to get all the canals? Those are really important things. I’d like to know is there a LEO on the film? If you had a LEO earlier than here, did it already heal or is it just kind of hanging around and there’s no apparent improvement? So these are all things.
Sometimes I’ve said to a patient, I don’t know; let me try one more thing. Your doctor I know wants a post space, because the caries is pretty aggressive and in order to clean it out, we’ll probably do a core buildup, and it might require a post. If I’m using a hot instrument and I plunge into one of your canals, like say the palatal root of an upper molar, what do I smell in my mask? And as you know, I know, every dentist that practices knows; breaking down root canals have putrescence, it fills the operatory, and the decision is in. We’re not going with this endodontics; it needs to be repeated.
Okay.
So those are some of the things.
Now I guess if you were looking at a radiograph and you saw kind of a dark area in the pulp chamber; maybe that’s your case that you wanted to bring up and talk about? Because this is maybe a sure thing you should probably retreat.
All right, so I can go really quick on this. So we have a case here, Ruddle’s – I’ve said this, but most of the patients I see have already had endodontics. So this is not my case, this is my preop, it was done some years ago. And as you can look at this case, you can begin to immediately see it’s ledged. There’s a big shelf. And there’s a little squig of maybe material trying to find the physiologic pathway. But it’s well short and it’s not endodontics as we know it. It broke the rules of symmetry and there’s a frank lesion.
So Ruddle went in really quick without any discussions. Look at all these composites. You can see all the composites are black; that was an era of dentistry when the composites were radiolucent. But they’re pretty much circumscribed; not like ragged and cariously aggressive.
So I went in and I retreated. That’s my anchors away case, just for your information; I was very pleased with it. And I put a cotton pellet in the chamber as I did in the 70s, and then I put Cavit above that. And I said you’re good to go; go back to see your general dentist and have it repaired. And so they came back to me on my six-month recall and they said well, we didn’t get back to the dentist. Something feels rough back behind, maybe even a little hole. And I’m looking at it and this is what Lisa was asking me on the previous question; what do we do now? In this case it was – oh, forget this case. This is just a problem leaving cotton pellets in the chamber. Let’s just stay there.
The bone healed. You can see if you look carefully at the third image on the right; the bone is repaired. I’m six months later, but we said 20 days. So when did it break the Cavit? I don’t know. They’re asymptomatic. The film says bone filled. Are we just going to put a crown on it? Or are we going to --
So what I would say is, okay, money’s always an issue for most people, so let’s be kind. Why don’t we just get them back to their general dentist with the understanding do the definitive restorative. But at some point in the future, we may have to go back through everything and retreat it. Because I wouldn’t want to do an apicoectomy on that surgically, because I’m just addressing the little part of the canal here. But if it’s leaking stem to stern I’m worried about that.
All right. So then if you have a tooth with recurrent caries, and it looks like you take the crown. You’re looking at the radiographs say, and you think you see a cotton pellet. Then that would be a sure sign that you should probably endodontically retreat that tooth. That it’s just not enough to clean out the caries and --
I think so. And remember, dentin isn’t solid. Even at the CEJ there’s about 60,000 dentinal tubules per square millimeter, so microbes easily fit into a dentinal tubule and they can move through tubules and get deep into the chamber.
So my Cavit in the middle image is blocking the access cavity; it’s protecting it. But when they lost the Cavit, all bets are off, because you’re right down to a cotton pellet which is almost like a wick. It’s like a sponge, it’ll soak stuff up.
Okay. Now what if the endo looks good and the patient’s asymptomatic? And that’s kind of what it was in my case. So is there anything that you would be looking for, maybe on a radiograph, to make you think that the tooth probably didn’t need to be endodontically retreated; that simply cleaning out the caries and maybe replacing the crown would be enough? Is there something that would make you feel pretty sure that the endo is protected?
Well I think you’re bringing up the heart of the – the meat and the potatoes. Orifice barriers. So intercanal orifice barriers. OB, orifice barriers. There’s a lot of different materials. I went from a cotton pellet to amalgam. Then I went to bonded amalgam. And I would put that 1 or 2mm below the orifice.
So I don’t want a barrier to extend deep into the canal, because what if? What if they break their tooth? What if they need a post space? It’s very hard to drill out amalgam to mid-root. So always think what if? What if they break the filling, what if they need a post space, what if? So leave an out so there’s a fallback position.
I want you to know though; a lot of times today we’re using polymers. So we’re using resin modified, glass ionomers. Gordon Christianson talked about resin glass ionomers that could release fluoride. So these are caps that go over the gutta percha, and they’re like – I said 2, but I like 3 or 4. That would take you to the coronal one-third. Every third – coronal one-third, middle one-third, apical one-third – every third is about 3,4,5; 3,4,5; 3,4,5; average is 4. So no more than 4mm below the orifice, and there’s many materials. Be careful with curing lights, because there is some shrinkage during polymerization and we have to be aware of that.
So I still like the tricalcium silicate cements. So that would be like Biodentine in the modern era, MTL. I like Biodentine now because it’s easy to mix, it’s more putty, it’s pressed into place, and that protects your gutta percha.
Okay. Well probably if you’re really working hard to seal off the canal with a protective barrier, you should be communicating with the general dentist to find out how they plan to restore the tooth; to make sure you don’t really seal it off when there needs to be a post.
You know, I’ve said this. But you almost need to have like an MO, a modus operandi. Everybody you work with, whether it’s a he, she, another country; take responsibility through great communication.
Like in this case. You wanted to see one with a barrier? So they come in; again, most of my cases are retreatment. So it’s failing first bicuspid. Everybody in the room that is watching this, in your house, in the office, wherever you are. If you’re jogging, you’re probably not watching. You see a silver point, and this tooth is rotated a little bit, so you’re seeing the buccal/lingual dimensions. And it’s hard to imagine that a silver point could fill a maxillary bicuspid root canal system.
So let’s not go into too much. You can see there’s fillings everywhere, patchwork. Notice all the patchwork that we as dentists do. When should we stop doing all the patchwork? I know you’re trying to save money; I get it. But risk versus benefit.
So I get the silver point out, I find an apical bifidity, I down pack into the bifidity. I have other views I didn’t include because of time, but I’m right on that apical septum with my pluggers, and I can get a thermal softened wave going buccal/lingual. So I was very happy, back packed, and then I put a bonded amalgam barrier off the gutta percha all the way to the top of the tooth.
And that was really important, because guess what? They came back for their six-month recall. Notice the apical healing. Notice the bone inevitability to regenerate when microbes are removed and the seal is effective. But notice the filling in the distal, the third image; the distal amalgam fell out. There’s now recurrent decay. And as bad as that is, it’s at least blocked by my alloy barrier. So that’s second case talking about the importance of a barrier.
Okay. So here, probably just fixing these caries would be enough because you have such a good barrier that you’re not really worried about the gutta percha.
This might be like your case. You know, where your bone – like we never talked about was there a lesion or not, but you were asymptomatic. Well if we had a previous film and you had a lesion, and now you don’t have a lesion, and now you’ve lost the filling and you have more caries. Look, it’s healing. I don’t think we would redo the root canal. I think we would say run, don’t walk, to go to the dentist.
Okay, so what about this scenario? So maybe the clinical findings seem to indicate that the root canal is leaking and should be retreated. However, a grim history of caries has eliminated too much tooth structure for the tooth to be restored. So probably then you don’t just gung-ho go into retreating it endodontically, right?
You know I love that question because it reminds me of the AAE Discussion Forum. There’s been some really nice efforts by clinicians doing caries control. Remember, we do this all the time; whose job is it? Well if the general dentist refers it in, clean out all the caries. Don’t leave the caries and somehow line it off internally and say I could do a root canal perfectly; now we’ll let the general dentist be responsible for the rest of the seal. Let’s make sure it’s restorable.
So as we’ve watched over the last two or three years, there’s more and more exotic carious cleanouts. I could mention apically repositioned flaps and osseous recontouring, crown lengthening. I’m not talking about crown lengthening; that comes to mind immediately. But they’re doing exotic stuff where they’re close to the crest of bone. I want to say biological width; you’ve got to have it. From the depth of the sulcular attachment to the height of the bone; that distance is the biological width. It’s got to be at least 1 or 2mm. And then we’ve got to have a ferule effect.
So I see these guys doing this great cleanout. One guy – I won’t mention his name – fabulous operator; we’ve talked about him before. He’s in the lower molar, he’s in the buccal furcation, and he’s barreling back towards the lingual; the caries keeps going. And he’s doing this exotic thing. What do you think Ruddle was thinking? Hemisect the tooth dammit! Because if you hemisect and bicuspidize that molar, now you can slap floss through there, they can get a margin, the furcation – the furcation floor was high. Here’s the bone. If you have a furcation floor that’s way below the bone, you can’t do that. But if the furcal floor is right at the height of bone, it’s a perfect tooth to think outside the box. But see we don’t think about hemisections and that’s why we do that segment. We’ve done a couple of endo/perio. We even had a podcast. You’re all watching RUDDLE+ so you could see endo/perio twice; once on the show, once on the podcast.
So in that case, you’d extract the tooth. Get rid of the tooth, paste an implant or a fixed bridge, or a free distal extension.
That might be easiest for the patient; you know, from the patient’s perspective. And they might not want to go through all this creative treatment to try to – I mean at some point, you’re like maybe it’s just easier to extract it and have an implant.
A lot of it’s just how you talk with your patients; your confidence level, who’s on your team, what kind of work have you delivered over the past years. A dentist may see this as huge caries. I’ll get all the caries out, cut the tooth in half, two crowns; that’s not so bad. Talk to your patients and explain to them.
So when I do this chairside, I have to give them all the alternatives. Your tooth’s really been - you’re a great patient; you’ve tried so hard. I can see you’ve had endodontics; it seems to be working. You’ve gotten – you had a crown on, but you’ve had several crowns before that. So this patient has put a lot of effort into this tooth, and now they have massive decay. To her point; if they had a history of a lot of caries, why would you be able to do such an elaborate restoration and this time it’ll be different? Maybe it’ll be the same mouth, the same person, the same hygiene, the same everything; so maybe it’s best to say sorry, I can’t help you.
But a lot of times as you talk to patients about well we could extract it and do an implant, we could extract it and do a 3-unit bridge if there’s a distal abutment, we could do a partial denture – in and out. And you give them the price, the time and the prognosis for all the alternatives; a lot of people will come right back and say you know, let’s give it a whirl and see what happens.
I think I find myself always asking when I’m given options; I always ask the clinician… Well what would you do if it was you? Because then I kind of get a better idea of like what they think is best. Without – I don’t know; I ask that question a lot. Like what would you do if it was your kid; or what would you do if it was your tooth?
I think if you must speak, it all starts by asking questions. Questions are the answers. I agree.
All right. Well do you have anything else you want to say or emphasize?
Well I wanted to bring a case up, but I also wanted to talk about Denny Southard. Denny Southard’s an old pal of mine, and he wrote a really good article in Practical Periodontics and Esthetic Dentistry, 1999, so he’s a little after the 85-91 or 92 window. And he came out with immediate core buildup of endodontically treated teeth; the rest of the seal. And I love that, because Denny, I’ve used that line so many times around the world and I always say that’s my pal, Denny.
But we always worry about the endodontics; we’re always trying to get really great cleaning, great agitation, great exchange, filling root canal systems with rubber and sealer complex. Okay, and then there is the rest of the seal.
So Denny wrote a really great article about that. And then I liked the Ray and Trope article. Martin Trope – everybody knows him in endodontics – and Ray, they wrote an article in ’95. And listen carefully… They said that a poor root canal with an exquisite restoration is pretty good; it works pretty well. Lousy endodontics and the rest of the seal.
They also showed that exquisite endodontics with a lousy restoration; it melts down because of this 20 – hey, who cares if it’s 20 days, 22 days, 60 days, 90 days? Are you getting the message? When gutta percha is exposed to oral salivary components, it breaks down in a very short period of time, and that’s the message. And I think I’d like to show this case.
Yeah, I actually thought it was interesting. Actually poor endo with a good restoration has a better prognosis.
That’s right.
Than good endo with a bad restoration.
And here you go.
Wait. Did I say poor endo with a good restoration?
You said it right.
Is better than good endo and a bad restoration.
Right. So this patient was sent in for the second molar. Let’s not get into too much – has a massive furcation blowout, apical pathology, pins everywhere, come on. And then look at the – there’s no discussion about the molar anterior. And it’s bridge abutment. So there’s a lot at stake with this because it’s carrying a 3-unit bridge, there’s massive caries under the margin of the crown, it’s already had patchwork fillings, you can see the patch, and it’s an old root canal tooth and it never hurt. So the patient never came in and said it hurt. They came in because the second molar was pushed up in the socket; every time they bit down it was like terrifyingly painful. And of course the second molar you couldn’t even touch it.
So they had two separate, distinct and unrelated problems. I said we’ll do the second molar; let’s go ahead and do it. But remember, we have another issue and I can’t tell you how much of your pain component could be coming from one versus the other. Maybe a little bit of both, but let’s do the obvious. So I did, and I said be sure to – I’ll tell your general dentist, we’ll talk about it. So I called up the general dentist and I said you know, we have two separate and distinct problems. I’m going to do the root canal and then he’s going to come back. Maybe you could take the bridge off for me, put a resin provisional bridge in there. I’ll take that off, I’ll get that silver point out of the distal. He was talking me into leaving the MB and the ML silver points because it was a long time ago and there’s no lesion at the end of the root.
So we did the root canal and I was very, very pleased. You can see this is immediate post-op, and I’ve got good anatomy, curvatures and all that. So I said okay, we’ll get you scheduled and we’ll have you come back and we’ll now – your dentist is going to take the bridge off, put the resin bridge on. And then I’m going to take out – we’ll at least do the distal, because the distal canal apically has a frank, obvious radiolucency.
So I saw him in six months. The dentist removed the caries. He cleaned out under the bridge, he must have made a remarkable seal because notice apical to the silver point. Ruddle didn’t take out the silver point; Ruddle didn’t retreat the canal; the canal is obviously teaming with microbes. But he cut off the food source.
So we’re not perfect out there are we? So the idea is to reduce populations from a massive amount to a more manageable amount that the immune system of the body can handle, but this shouldn’t work. You know I did a segment a while back, Tooth on the Floor. You wouldn’t think those things would work. You wouldn’t think that would work. Now maybe if you had CBCT they would say oh, I see something. But you know what? By cutting off the leakage coronally, the endodontics is working.
So this is not what I’m recommending. But even in spite of us, sometimes things work.
Well I can kind of now understand a little bit more why endodontists might be sensitive to GPs leaving a cotton pellet, or maybe not emphasizing to their patients the importance of an immediate restoration. Because it’s their work that’s at stake. They don’t want their work to fail so they just want the seal to be finished so that it can be protected.
That’s it. So what is a triple seal? I never defined it, did I? Triple Seal! You’ve got an orifice barrier; put up a finger, that sounds like one. Then off of that you bring a core buildup right through the access cavity, or maybe rebuild a wall; you know, matrix bands, ortho bands, two. And then you cut your preparation, you get the ferule effect, you put a crown on that, and that’s a triple seal. How about that; a triple seal.
Okay, well thank you for this information and that’s it for this segment.
SEGMENT 2: Transport Types 1-2-3
Welcome! Listen, I’m very excited about this topic specifically. Because we’re going back to the old game of clean and shape. And then we do that so we can disinfect. So shaping facilitates cleaning, and shaping facilitates filling root canal systems.
However, in the shaping game we’ve talked about meticulously negotiating canals. And once we have a secured canal, which means a smooth, reproduceable glide path, then it’s just down to an appropriate root-appropriate shape. And the shaping has been a little more controversial in recent years, because we have minimally invasive people. I like to think that my camp, our camp, most of you out there watching this; we want root-appropriate shapes. Because really, the shapes are the flow path; and the flow path is our 3-dimensional irrigation concepts that lead to clean root canal systems.
So during this exercise of repairing canals, even though the files have gotten a lot better, we’ve moved to NiTi, then there was heat treatment, and then there was a whole range of heat treatment and it’s still going on. We want more flexibility, especially in root curvatures.
So if you look at this molar and you think about this as your preoperative film, and you’re thoughtfully looking at it just before you pick up the handpiece to start your access cavity; right, that’s what you’re doing. You’re getting oriented, you’re beginning to start with the end in mind, you’re beginning to see how the gutta percha is going to flow and you’re beginning to see maybe lateral anatomy. You don’t see the lateral anatomy on well-angulated films, but you might see a lateral root lesion with an intact sulcus, and that speaks to a lesion of endodontic origin.
So let’s get this in motion, now that you’ve got it absorbed thoughtfully chairside. One last look before you access and you’re looking at the breadth of those roots. And you might even be able to see multiple systems, and you’re beginning to start with the end in mind.
So most times today in posterior teeth, if you’re the first one in and the last one out endodontically speaking, you’re going to have perimeter diameters of 20, 25, or 30. Many different file systems that do this. I’m showing ProTaper Gold; it’s still the most sold file in world after all these years. It is a beautiful set of instruments; you know that, I know that, we all know that. And then some of you had to go to cheaper files because you thought you could save some money. But there are no exact copies of ProTaper, because the biggest files are 6%, not 7,8, and 9.
So this would typically take care of most of your molar teeth. You have heat treatment, you have gold, you can get blue wire if you want to go ProTaper Ultimate. And of course some of you even still use stainless steel hand files, that’s fine. But you’ve got a nice, flowing shape. Schilder would have classified this as the mechanical objectives or a funnel-shaped preparation. Maintain the original anatomy, maintain the position of the foramen, keep the foramen as small as practical.
So that’s kind of what these files can do. They can snake around multi-planar curvature. And we have a foramen and it’s positioned exactly where it was on the external root surface. So after shaping, we haven’t moved the foramen; it’s just a little bit bigger.
Well what happens though a lot of times because of shape memory, files want to get straight. They’re manufactured straight, they’re always trying to straighten back out. As you go around the first pass with your file, it has dentin holding the file, keeping it centered. If you go back again and again and again, the hole’s getting a little big, bigger, now the file will begin to ride on the outer wall. And as the file rides on the outer wall, you’ll begin to see the interesting rip. You can begin to see the physiologic foramen has been dragged to a new iatrogenic location on the external root surface.
So this causes problems. And the problems show up right now in shaping, by the Type 1 then is just a minor movement. So we don’t like any movements, but a minor movement is better. Now I’ve talked about Type 1’s on this show, and I’ve talked about Type 2’s, and more than one time. And I’m reviewing it again, because my real assignment today is Type 3’s. But Type 3’s are typically surgical corrections. And we’ve talked already quite a bit of surgery, but those of you that have gone to RUDDLE+ know that there’s a surgical continuum. And we’re going to have about – I’m making this up – we’ll probably have about 25 or 30 shows when we’re done. We have maybe 6,7,8,9,10 posted. But we’re not going to go into all the surgical stuff in the detail that we would in the continuum.
So what we were taught back in grad school at Harvard is Schilder introduced the word “transportations.” He said when you have a transportation in that era we were using 02 tapered hand files. And the only way you’d know with 100% certainty that this is the file that’s snug at length – say it – snug at length. That means you can tap on the yellow handle, the 02/20, and it won’t displace. That’s after you’ve done all your body work. That means the foramen is more or less equal to the size 20.
If you get all your shaping done and you tap on the 20, and it goes brrrp – goes through the foramen – it means that you thought the 20 was snug at length, but it was loose at length. That means how big is the foramen? Well the key thing is if you have shape, if you have shape above the foramen, then you can introduce an 02; an 02 tapered 25. Is it snug? Is the 30 snug? And you can keep playing this game.
And as you play this game, you’ll begin to discover how big it is by inserting the 25, maybe the 30, maybe you go to the 35 and now the 35 is snug at length. It’s only snug at length if the 40 is back a half a millimeter; that’s about a half a stop. And if the 45, another half -- 50, 55, 60. Like going up a stairway; the rise is the same on each elevation on the stairway so you don’t fall.
Well so you don’t fall endodontically, we want each larger sequential instrument to uniformly back out of the canal. Then when you tap on the handle of the file that’s at length, it’s snug at length and you know you have resistance for your irrigation. This is what holds your reagents, it prevents sodium hypochlorite accidents, and also good exchange so that we can pack in three dimensions. We’ve got a capture zone to hold thermal softened gutta percha. So that’s what you’re trying to do.
Well if you look at your root and the 35 isn’t snug and it’s loose, that means the foramen is bigger than a 35. You might even go bigger; you might even think about how big can I go? We’ve got a thoughtful look at three well-angulated films, maybe you have CBCT ; start looking for root bulk and form, and begin to ascertain can I safely – risk versus benefit – can I take the foramen a little bit bigger? Can I go a little bit larger so I have a capture zone?
Fortunately we don’t have to use all these files. I mean I still like the 02s to gauge; we’re talking about gauging today. And you can go back and look at several shows and we’ve talked a lot about gauging. So we won’t do it today, but gauging is confidence. Gauging is how big is the terminus?
So we have a ProTaper Ultimate, 35/12, out of blue wire. So the taper is 12%, only in the front end; and then it has regressive tapers, regressive percentage tapers. It’s only 12%; that’ll give you your capture zone. And you can use one instrument instead of boom, boom, boom – a lot of instruments. And it’s hard to teach colleagues how to very carefully make sure each larger instrument is a little bit shorter than the previous instrument. Most times you give a colleague a file and they want to take it to length, and you see them start to screw it right down, they seem to think that all files need to go to length. It’s a discipline; it’s an art form to back each larger, successively bigger file out of the canal.
So this is an instrument that you might think of that you haven’t noticed. Dentsply Sirona makes this, but they don’t market it because they made a secret file, just for secret people.
All right. You can even go in with a – okay, that’s the Ultimate. It’s the auxiliary large file. This is the auxiliary finisher, so we have auxiliary shaper and an auxiliary finisher, and we have two sizes, 50/10. Notice the flutes are only the first 5mm. This gives us a great capture zone. And even if these are NiTi, these hand files; when they get to be like 50, 55, 60 at D0, these are stiff. You can go to Sears and Roebuck and buy them right off the shelf of your friendly hardware store.
So we got pretty flexible with the ProTaper Ultimate auxiliary finishers. So be thinking about a 35 and a 50 if you need them in certain cases, especially in kids. We’re doing a lot of regenerative stuff on – anterior teeth come to mind --accidents and stuff like that. So now you have some really flexible files and they can give you capture zones.
So that’s about as big as we can go with a Type 1. You know, when the rips start to get bigger and the 60 falls, and that’s as high a file as I have in my office, you’re going to need another idea. So the other idea is to recognize this is the physiologic terminus. This is where it was spatially; it’s been opened a little bit by your work. This would be of course your Type 1. And then this is another one; this is a Type 2.
So a Type 2 is just a bigger movement; that’s it. But the reason these aren’t in textbooks, these types and classifications, but I classify them because it tells me what to do. So Type 1s are more minor movements. And if I can get shape above the foramen, I can treat it like a regular case – clean, shape and pack.
When they’re bigger, I’m going to need a barrier. And a barrier does two things, because these things are usually wet. That means it’s going to bleed, it might be clear, might be serous, might be purulent. But they’re rips. And these are rips and tears and foraminal relocations, and there’s usually wet canals. So you’re going to have to think about how do I block this kind of a diameter?
This is huge, and the pinch point is way back here. So what are you going to do in here? Well this is a great place where we could flow mud, like concrete or cement, and have a barrier down there to pack against. So what does a barrier do? It gives us a backstop to pack against so we have control; and it also reduces hemorrhage and bleeding and wet canals. We don’t want to do submarine endodontics; we want to be working in a nice, controlled environment.
So we have a bigger rip. And we’ve talked about these and I’ve shown you animations in different cases. Today I found an old case in the library; I actually found it a few days ago, a whole section of this stuff. But this is a CBO case; this is a carrier-based obturator. If you look carefully, you can see the file-like carrier with the circumferential gutta percha. You might think that’s a fragment of a broken instrument, but then if you look carefully, you can see in the other mesial system, it also has that file-like – remember there were files in the late 80s and then we went to polysulfone; that was a plastic core, a polymer. And then now it’s Guttacore – it’s a different formulation of gutta percha. So the carriers that Ben Johnson, Dr. Ben Johnson launched, have evolved and they’ve gotten really quite well. But the old ones that were done late 80s to early 90s had a metal file with circumferential gutta percha.
Well if you look carefully – we’ve talked a lot about these short fills. And I see something over in here; I see something over in here. That kind of maps the anatomy out. I don’t know if I’m going to have a branch here; I don’t know if this is going to turn like this with a lateral offshoot; I don’t know if it’s an equal employer opportunity. But I’m expecting something interesting in the distal.
And then I’m noticing that the geometric apex is right here. So why is the file moving around like this? As the bigger files come in, they’re stiffer and they begin to relocate. You can even do a transportation with a small file if you go back lots and lots and lots of times. You can get transportations if you run long in curved canals. Once that file leaves the root and starts heading out into the bone, if you don’t know that your working length is shortened, then your file in more curved roots is going to appreciate that the working length is going to decrease. And if you’re not backing off your working length, your WL, you’re working long and that’s where the rips really become problematic and they become quite big.
So I’m telling you a little bit more than about just transportations, aren’t I? Aren’t I? The teacher always teaches what he most needs to know.
So lots of things have been used to pick up MTA, so we’re talking about what would be a barrier material. MTA comes to mind immediately; we all worked with it starting in the mid-90s. It’s got more papers written about it than any other restorative reparative material in endodontics -- hundreds and hundreds of papers and now there’s been look-alikes and copies, different things like that. However, it’s still a great material because it’s like concrete; which means it’s loose, it’s in a runny mix, and you can move it.
So here’s how it comes. You can mix it, you can wick it, go to other shows to figure out how to get the perfect consistency. You can load it in a spinal tap needle or any kind of a micro tube. But most of you are going to want the Maillefer, Dentsply Sirona, the messing gun. It has these different gauges, you can see the stripe there in the red and the blue. Different size canula is what that means, and these screw on and there’s an internal plunger and you can see it sticking out barely at the very end; barely. It might look red to you if you pushed in really tight on that.
All right. So you pick it up, the MTA, and you pick up 2-3mm, a little aliquot, and you inject it and leave it in your shaped canal. We’ll pick up another 2 or 3, put another little one in; there’s your second one. Here’s our first one. And here’s going to be our third one; here’s our third.
So you have these little aliquots in there; they’re just laying loose in the canal. And so what I want to introduce is don’t put in too much. Or when you get on it to push, they’ll all kind of aggregate together, and as you push with a plugger, you’ll squeeze out like a sponge the moisture, and now it’s locked up and it won’t move. So go to other shows – see how I’m teasing you? I’m not going to show you everything in 20 or 30 minutes. Dehydrate, rehydrate. Learn how to rehydrate, very, very simple; but you’re going to use this to get it roughly in the middle one-third. It isn’t necessary to try to place your MTA exactly at the terminus, especially in curved canals. Just get it deep, about in the middle of the middle one-third.
Okay. Now take your gutta percha cones, your master cones, and you can saw them off with your scalpel or scissors, and you can make a very nice diameter. We want a cross-sectional diameter at the end of that cone that basically is the size of the canal – short. And that means when you feel a little resistance and you have your working length matched so you know your working length is way down here – you can see how this comes down and swings out, swings up. This is a big rip, this is a tear, this is a zip, this is a transportation. So trim the cone so you have something that doesn’t just stab into the loose concrete mud, MTA. You want to get on top of it so you can shepherd it.
So you trim the cone that’s appropriate, and here’s the bottom of the cone right here. And you can see now I’ve tightened up all those little pellets. Maybe you rehydrate/dehydrate again. But you get it into the target zone; that’s all you have to do. So you’re just moving it a few millimeters to get it unadapted, imperfect, but in the target zone.
What you can do now is you’ll hear this thing, it’s a little hummer. But this is the new SmartLite Pro EndoActivator, but it’s a polymer tip, so it’s not going to scuff more, ditch, ledge, break, all those things internally. And it can move this material laterally and apically. And even though there’s reversed apical architecture, usually when there’s lesions here, these lesions are empty osseous bone cavities; they usually have cystic material in them. More commonly most often, it’s granulomas tissue. Which means you have granulomas tissue in here.
If you just float – think of the word float. If you just float the mud down, you’ll have a marvelous adaptation as it just begins to move in, held by the granulation tissue; which you know from surgery is very soft, right? You scoop it out with a curette. I used to be able to pack it with a plugger, and I was pushing a lot of MTA through the foramen until we learned that vibration was the secret, not the packing.
All right. So we went from that to this. And I think you would say it’s a pretty nice recovery. We got this little short carrier out, there was a big transportation, if you look carefully, you can kind of see the shadowing in here, kind of see that. I’ll get these out of the way and you can look again; you should be able to see that. And how the real canal was actually the real pathway with the physiologic terminus – I’m a little high, but it was right in there. And you can see we’ve just floated mud all in this region. And then you can – we’ve talked about barriers, right? You can see we’ve stubbed a little barrier there, that’s an alloy barrier in that day. There’s a little – you can barely see the radiocontrast; you can see a little more opacity.
That’s my triple seal. I’ve got a crown, I’ve got a core, I’ve got a crown and I’ve got a barrier. That’s a new word for you out there; it’s a new word for me, I just coined it. Triple seal! You hear it first always here, don’t you? Triple seal. Did you hear about triple seal? Start talking about it. Maybe you’ll write a paper, triple seal.
And get him back on recall. Because you want to see how it’s doing. And notice how that bone is coming in. All we’ve got to do is change the biology, remove the microorganisms as much as we can – probably not in every instance, right? Even with advanced techniques of agitation and exchange of solutions. And then get a seal; and we know that MTA is a great material because it’s not so influenced by moisture. So we don’t want runny blood filling up the canal, but a little moisture helps the MTA set.
So when you put the MTA in here, you’ve got moisture on the external side when you put it in. And then we’ve got to put cotton pellets up here that are wet. Cotton pellets are against it, so the moisture requirement is fulfilled on the coronal side. That means two visits, so I didn’t show you all the documentation, but you’ve got to come back, take out the cotton pellet. If the material is soft and hasn’t set up, flush it out and do it again. We’ve talked about that in other shows, so I won’t really go through that again. Usually the first time it works, but if it’s not set up, there’s probably just too much inflammation; it’s too acidic and probably you need to change it again. MTA’s pH is very high, more than 10; acidic reactions are down here about 1. So you’ll be very successful on a second visit if you have to place it a second time.
And then we’ll finally get to a 3. So when you get to a 3, you have a massive rip. You can try to do a little bit of shaping, but the problem is you’re going to blow out the root trying to make this the narrowest diameter with greater diameters above it. So that’s not going to work; you’ve got to have other ideas. And what comes to mind is oftentimes I will go through the top of the tooth and orthograde and reclean and shape and pack the best I can, just to make sure the environment’s good, there’s no missed systems off the floor, no cracks, nothing’s leaking. I want control of the case.
But if you don’t do nonsurgical retreatment, you will do surgery. So what I’m doing is ortho surgery where the top’s open, the bottom’s open, and I have more control of the final outcome.
So on 3 is there are big rips. And you can see here, this is the world’s second biggest post. The first biggest post was placed by the same gentleman just a few years earlier and he shattered all the Guinness endodontic records. And now we’ve got the next post in, very, very big. It’s a screw post, it’s threaded. It’s a screw post for the service it provides the patient. I hope that works internationally.
So you’ve got a big lesion. I’m reading the root; it’s coming around here. I can almost track it. I’ll get all of this out of here, but you can see a little more shadow there. It’s coming around as it’s been ripped and ripped and ripped. So we’re going to go in. Got to reflect a careful flap; there’s quite a ridge of bone here, quite a bit of ridge of bone. We’re right below the crown on the mesial root, so we start our little window. You can see the granulomas tissue that I was just talking to you about how we can float our mud. I’ll get that X out of there, but you can see how this granulation tissue would serve to be a gentle, accordion-type backstop, if you don’t pack if you vibrate.
So here we are with a little bit more osseous work progressively uncovering bone. You can see that root’s been mutilated. I’ll do two of them. I see this line – do you see that – and I see this line. That’s like my fingertips; that’s the mesial root. The stairstep root. I see that the MB is right here. The canal comes down like this and it should have gone like that. But it didn’t. It went right out the side of the root because they ripped it. And if you look down here deep, you see the cone; but the root foramen is over there. So both of these foramina, in vivid detail surgically, you can see the iatrogenic work right up close through the microscope at X power – whatever you want.
So we get the root apisected, crypt control. We’ll talk about all this in surgery. It’s already done, I’ve done my part. I did something like 25-30 segments, and now we’re just populating the website as the demand comes. And we’re getting great demand on RUDDLE+, so thanks for coming over there because that’s where there’s more advanced learning and more of a dive into the pool if you really want to get below the surface of the water and see what’s down there.
So then you look at this think in the post-op. And you can see where the lesion was. I’m pretty close to the board, but it’s a pretty big lesion. So it’s nice and black here, we’ve cleaned it all out, apisected the root, crypt control, retro placement, and then let’s watch the bone work. Let’s watch the bone work.
And endodontics is predictably successful if we can remove the etiology. So today we had a little talk about transportations, 1’s, 2’s and 3’s. They get progressively more difficult to manage. You can clean, shape and pack on the 1’s if you can get shape above the foramen. Be careful you don’t mutilate the root though in the process, because there’s another idea. Type 2; have a barrier. I like MTA, especially internally to the top of the tooth.
Well 3’s will come up. Either be prepared to refer and have a good relationship with your specialist in town. Or maybe you’ve trained up and you can do it yourself. But whenever you can, let’s save some teeth.
CLOSE: Grandkids – Noah’s Tennis & Fitness
Okay, so we’re doing another grandkids segment, and probably most of you are aware that my parents have five grandchildren; two from me and three from my sister, Lori. And you’ve seen them make some appearances on The Ruddle Show over the seasons. Our plan was to feature one grandchild over the seasons to find out what they’re up to and see what their interests are at this point in time. Because you know what they say about grandkids. They restore our zest for life and our faith in humanity.
So we’ve already met my daughter Eva and my son Isaac, who you know also works on The Ruddle Show. And then now – and we talked to Sophia, Lori’s middle child. Now we’re talking to Sophia’s older brother, Noah. And we’re going to talk about tennis, training and total body health.
Hi Noah, welcome to the show.
Hi Lisa. Thank you for having me.
Yeah, I know you’re really excited about this.
Good to have you on the show, champ.
Thanks, Papa.
All right. Well we have some questions for you, and there’s a lot. I might not get to all of them. But let’s just start with what keeps you busy day-to-day?
Well I’m a tennis player first and foremost. So whether it’s on the court, off the court, a lot of my energy is going towards becoming a better tennis player. So yeah, a lot of hours on the court, in the gym, in the pool, and tennis is my passion.
So you do some cross-training?
Yeah.
Okay, that’s nice.
I run into him sometimes in the other area of his life, the gym. I think he’s a gym rat.
You're always in there before me though.
(Laughter) He’s in there before Noah and after Noah. So how much time do you spend playing tennis a day, about?
It ranges, but probably at the peak of my training, it would be 4-5 hours on the court, and maybe a couple of hours in the gym.
Is it combination matches and then just practice? Do you do ball machine stuff too?
Yeah, definitely. I kind of – I listen to kind of what I need that week. Or if I’m in a tournament, I might do more match play to get myself prepped for that. Or if I’m working on more technical things, I’ll use the ball machine, hit with my brother and sister.
So this is not a question on the list, but I have this personal question. What’s your secret weapon?
Secret weapon?
In tennis.
I think my secret weapon is my obsessiveness and my attention to detail. That allows me, I think, to improve in all aspects of my game. I’m very determined to master tennis, so I think that can – every shot can fall into that category.
Okay, great. So has tennis always been your number one sport?
No, no. I was a kid that played a lot of different sports. I played soccer, tennis, baseball, basketball. And at one time or another, I was probably set on playing one of those for the rest of my life. But throughout trial and different teams, different – in high school, I came to tennis.
And what made you want to focus on tennis? What about it did you really like?
I love the individual aspect of tennis, and the fact that if I win it’s on me, if I lose it’s on me. I know exactly what I have to do. When I played soccer especially, I didn’t like when my team would win and I wouldn’t score. And I also didn’t like when I would score and my team wouldn’t win. It was that kind of dichotomy which I wasn’t a fan of.
So you kind of have more control over your success.
Exactly.
Your personal success.
You know where you went to high school, that iconic Peabody Stadium?
Yes.
He’s kicked some balls in there during matched plays, so that’s no small feat.
Yeah, I remember at one point it seemed like you were equally into tennis and soccer. Like it could have maybe gone either way for you.
Basketball and baseball went by the wayside a little earlier, and then it was between soccer and tennis. And yeah, maybe at times I thought soccer was the thing I was going to do, but it ended up being tennis. And I’m very thankful for that.
All right. Well my next question… How has your journey been? So what challenges have you had to face?
Well I mean it’s only natural when you're trying to achieve a certain amount of success and mastery of something that you’re going to go through challenges.
I’ve never had that happen. It’s been just easy breezy.
My perfect Aunt Lisa! But yeah, I’ve had challenges for sure in the form of just – I’ve tinkered a lot with diet and have run into energy problems; just trying to find what works for me. And luckily I’m a lot better off now having gone through that. But yeah, that was probably my biggest challenge.
What about injuries?
Injuries? I’ve had stuff with my back, my shoulder. I spend a lot of hours on the court, sometimes maybe too much, and those little pains have reminded me of that. But yeah.
Gosh. You know I actually have – I can relate to a lot of what you’re saying because a lot of my age around your age was tinkering with my diet. Overtraining in some areas and then getting injured and having to balance it out more. So I like the – so what’s the cross-training you do?
I like to – well one aspect of my training is swimming, which I’ve found has been really beneficial because there’s no impact on the joints. It just feels very refreshing and you’re also getting a workout at the same time.
What about your eyes? Does that bother your eyes in the water?
I wear goggles.
Okay.
No, because I learned my lesson with that, because one time I was swimming laps before class and I didn’t have any goggles. And my eyes were burning so much that I couldn’t really see the white board and what my teacher was writing down on it. So I learned my lesson there.
Okay, I’ve heard some comments from my kids when they have been hanging out with you, and they comment sometimes on the enormous – and with a little bit of jealousy – the enormous amount of fruit that you’re able to eat, to still be in this great condition. So what would you say is a normal diet for you in a day?
I mean I eat a lot of whole, healthy food. And so when you eat those foods, and especially with my activity level, you kind of have to eat a lot more. And so there’s nothing, no secrets.
Do you eat what you want mostly, and then try to put a healthy spin on it? Or do you ever go off your low diet or your way of eating and just splurge on something?
I have what I feel like. And so sometimes yeah, that might be like a burger or a pizza. But I don’t feel like that’s often, because a lot of time I feel like what’s going to make me feel the best. And luckily, I mean having a healthy diet there’s a stigma that it has to be bland and not taste good. But I mean I don’t really think that’s the case.
No, I also agree. And also I do notice myself – because I eat pretty clean too – and then when I do eat something different, I almost feel like my blood is more sluggish or something. I feel like it’s just not as efficient.
I have a comment.
Okay.
You guys have heard of Phelps, Michael Phelps, the gold medalist. He has so many medals I guess he has to build a bigger house. Anyway, him and Noah – Noah didn’t put it this way, but he tries to go for total calories. He’s thinking what he’s burning, and then he’s got to eat at least that much to have reserves – he’s got to eat more. And so I heard him the other day during the Olympics when they were interviewing him, and he said it was so tough to get – I think it was like – I don’t know. It was an enormous amount of calories.
Like 10,000.
I think it was 10,000. And they said well what do you do? You only have like 9,000. He said ice cream, chocolate bars, burgers, cheese. He said he just has to pile it on. It was hard. I think it’s hard for him. When we go out for dinner – this is a side story – we’ll all order. Like I’ll get a drink and everybody gets their little appetizer maybe. Noah will get like 4 or 5 salads.
I don’t know about that!
But they just look at him and they start bringing these plates. So it’s all very fun to watch. I mean look at him. What’s your body fat?
I don’t know.
What was it?
I don’t know.
It was a single digit number.
And what’s yours?
Mine is about 50%.
It’s too low, it breaks the scale. Unreadable.
Well I don’t know if you know this, but we’ve been talking a lot about legacy this season.
I’ve been hearing a lot on ESPN.
I know, I hear about it too. It really spurs me to talking about it. So who are some of your favorite role models or people that you admire -- with legacies that you admire?
My biggest role model is Novak Djokovic. He’s, in my opinion, the greatest tennis player of all time, and the way he carries himself on and off the court is something I really admire.
He’s vegan too, I think. Isn’t he vegan?
I don’t know if he’s full vegan, but he’s like I think predominantly. He doesn’t have much meat at all; he’s very like vegetable forward.
Yeah. He’s one of my favorite tennis players too. Well okay, he is my favorite tennis player as well.
Is he the greatest of all time? Just by the numbers?
By the numbers there can be no argument.
What about outside of tennis? Do you have a favorite role model?
Probably Cristiano Ronaldo, soccer player. He’s my favorite soccer player and I really admire him for a lot of the same reasons.
Okay, nice. So what about your legacy? What are you working towards? Like if you think 50 years down the road and someone’s talking about you, what do you want them to remember?
Um, that’s a good question. Probably just my all-around determination to master myself, master my game, master my body, master my mind. If I can do that, then many successes will come my way.
Well I really – the thing I really like that you’re doing that I’m hearing is the cross-training. Because when I think where I am now, and I do so many different things; the weights, the karate, just the training we do at home. I actually feel stronger now in totality than I did when I was your age. And now I think if I knew now what I knew then, I could have been a contender. That’s what I think. So yeah, you’re doing great with the cross-training. I really – I try to get Isaac to do a lot of different things too. We even do bar workouts, ballet workouts, because it's really helpful for flexibility and stuff too.
I’ve actually considered doing ballet and stuff like that.
Yeah. I would strongly recommend it. We just got into it in the last year, and I can’t even believe how much strength is required and how much flexibility you get from it too.
My mind was blown when I read Arnold Schwarzenegger’s book. I heard that he took ballet classes at the height of his peak because he wanted to get better at posing and become more fluid. Because obviously he has massive muscles; he doesn’t want to be too muscle bound and tight.
Yeah, that’s nice. And Jerry Rice, he also did ballet in the off season.
Oh, okay.
He sure did. And we started a whole trend in the NFL where people started to go train with Jerry in the off season. They’d run the paths and do the ballet and all that. He lived up in the hills and they’d go off on 40-mile runs; 30-mile runs and then they’d do the ballet.
Wow!
Well I’m having a lot of fun interviewing you. It could go on and on, but I know that this was supposed to be 5-10 minutes, so we’ve probably reached that. But thank you so much for coming on and telling us what you’re up to.
Thank you Lisa. Thanks Papa.
You know, one thing I want to say to the whole audience, our large audience around the world, is this kid has discipline like you can’t imagine. And discipline is going to carry you in any endeavor. It’s going to carry you to the top of your game. Not maybe the top of the profession, but the top of your game. And doesn’t smoke, doesn’t drink, doesn’t use drugs, eats really good food, and is he disciplined.
And has a great heart and is kind.
Faithful. So I’m predicting great things. Thanks for joining us.
I second that. Okay, well that’s all we have time for today. See you next time on The Ruddle Show.