"There is a well-known clinician and lecturer who is frequently introduced to dental societies as the man who has written more, published more, lectured more, and just plain talked more on the subject of toothache than any other man, living or dead. He stresses that..."
Cracked Tooth Syndrome & Resorption Endo History and “Through & Through” Management
The show begins with Ruddle & Lisette talking about some highlights from the recently concluded AAE meeting… from Ruddle’s unique perspective. Then, the duo travel back to 1968 to revisit an article by Harold Stanley; has our understanding and management of fractured teeth evolved in the last 55 years? After, Ruddle is at the Board discussing the management of “through & through” resorptions… is surgery sometimes indicated? The show concludes with a return to Demotivators, because we all love an occasional dose of sarcasm, wit, and irony… as well as a little reflection on LEGACY. Wait, what?
Show Content & Timecodes
00:16 - INTRO: AAE Meeting Highlights via Ruddle Texts 08:38 - SEGMENT 1: Endo History – 1968 Article “The Cracked Tooth Syndrome” 30:55 - SEGMENT 2: Management of “Through & Through” Resorptions 59:53 - CLOSE: DemotivatorsExtra content referenced within show:
Other ‘Ruddle Show’ episodes/podcasts referenced within show:
Downloadable PDFs & Related Materials
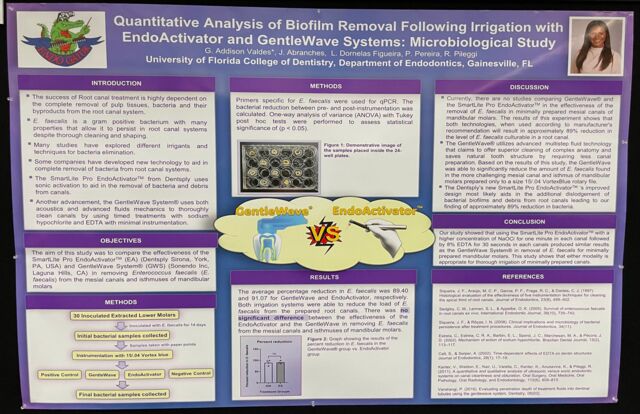
Summary Research as presented by Dr. Addison Valdes at the AAE 2024 Meeting
Dentists are trained to thoroughly review medical and dental histories and perform comprehensive extraoral and intraoral examinations. Yet, in spite of these efforts to optimally serve patients, the dominant clinical reality is...
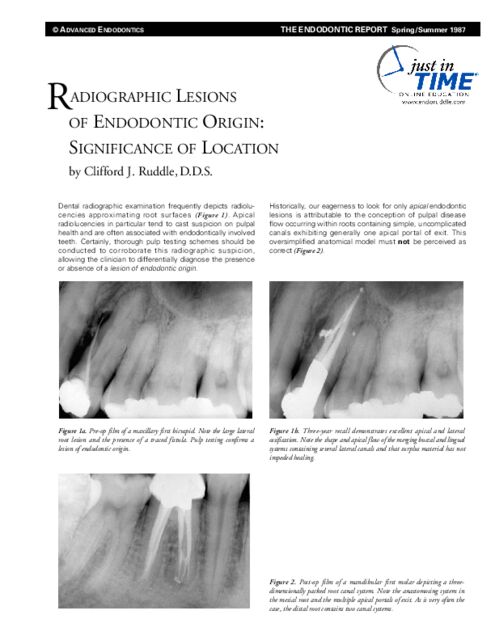
Dental radiographic examination frequently depicts radiolucencies approximating root surfaces. Apical radiolucencies in particular tend to cast suspicion on pulpal health and are often associated with endodontically involved teeth...
Mao Tse Tung wrote “The foundation of success is failure”. Clinicians who strive for endodontic excellence appreciate the elements that comprise success and use these criteria to evaluate the causes of failure. Endodontic failure occurs for a variety of reasons, but what all failures share in common is leakage...
This transcript is made available by The Ruddle Show in an effort to share opinions and information, and as an added service. Since all show text has been transcribed by a third party, grammatical errors and/or misspellings may occur. As such, we encourage you to listen/watch the show whenever possible and use the transcript for your own general, personal information. Any reproduction of show content (visual, audio or written) is strictly forbidden.
INTRO: AAE Meeting Highlights via Ruddle Texts
Welcome to The Ruddle Show. I’m Lisette and this is my dad, Cliff Ruddle.
How you doing?
Pretty good, what about you?
I’m good and I want to wish out everybody out there best wishes for health and happiness, and I hope your life’s going real good.
Okay. Well you recently went to the AAE meeting. We mentioned it on the last podcast we did, but we’re going to give you a little different perspective of your trip to the AAE meeting today in our little opener.
I just want to tell everyone that we are in a group text with my son Isaac, because we often work together, and we also have similar sports interests so we use that for sports too, that little group text. So when you were gone, you actually were texting us and giving us some updates on your trip. And it was kind of funny and humorous, and Isaac and I decided that we’d make a little keynote presentation to show your texts to us and what you texted us; to give your perspective.
I never realized those little text messages were going to become public.
Okay, so here is Ruddle’s unique perspective of the recently concluded AAE meeting as seen through his texts. So here we go. This was the first text we got, and the last text… (reads Ruddle text)
“Upon arrival - a glimpse of the jungle; upon departure: Big hugs to all. It’s good to have escaped the zoo and we’re glad to be home.”
So I notice that you referred to LA as the jungle and the zoo. Is that –
Well, when I look out my windows at home I’m looking across water, and I see distant islands and the city, and it’s quite peaceful. And when you’re in downtown LA and you throw your window open, you’re looking at one tower after another, so I thought it looked like a jungle.
Okay. Next one… (reads Ruddle text)
“Insignificant info; destroy if appropriate. This Marriott by proximity to Crypto.com Arena must be an official hotel where NBA road teams stay, I think? My assertion is based on the height of the shower ceiling and shower head – which seems to be at about 9ft off the tile floor. Although Phyllie had a very nice hot shower, by the time the water fell to her pedestrian height, she reports the water arrived cold. There will be other critical headlines from the Rudder on all things important.”
So you stayed close to Crypto.com Arena?
We tried to stay closer to the head of the shower.
Okay, so we got a shower update. The next one… (reads Ruddle text)
“Hey guys. Today outside the Crypto.com Arena, Mitch took my pic in front each of the fabulous dynamic bronze statutes of the Laker greats. Jerry West, Elgin Baylor, Kareem Abdul Jabbar, Magic Johnson, Shaquille O’Neil and Kobe Bryant. I felt a deep reverence for the game and these iconic players and their legacies. Wow!”
So the meeting was close to Crypto.com Arena.
Just literally as we walked from our hotel; they say when you get to the Y in the road, take it. A few steps this way is the LA Convention Center; a few steps this way is the Arena, Crypto.
And you were sort of pulled in the one direction.
Well, I had never actually gone to the front entry. I had never been to the Crypto.com Arena, so I was not going to be that close to it and not just see what was there. Over the years I’ve heard that this guy got a statue and this guy got a statue, and this guy; they’re arguing about the statute. So I thought gee, I want to see the statues.
Well let’s see what you saw… (reads Ruddle text)
“One of my favorites was Elgin Baylor; one of, if not, the first to play above the rim. He was art in action.”
You look very nice in that picture; very.
Well you know Elgin Baylor; I don’t know how to say this, but it just depends on generational stuff. Every generation has their iconic players, but when I was a real little kid, Elgin Baylor could do stuff in the air that was like breathtaking.
Okay, well here’s another one… (reads Ruddle text)
“Of course Jerry West was awesome and a deadly assassin shooter… Note the far background.”
Yeah, well he was known as Mr. Basketball. And also, those of you that are overseas, if you ever watch NBA basketball, he is the logo on the basketball.
Okay. Next one… (reads Ruddle text)
“In the above image featuring Jerry West – so in the one we just saw before – in the background, you saw Shaquille O’Neil. Here’s a little closer look.”
So you got a good picture of that statue.
Yeah, I was thinking he might just rip that thing right off the wall; because Shaq has broken some glass backboards over time.
Next one… (reads Ruddle text)
“Oh, some more pictures of you with the statues. The Captain, Kareem Abdul Jabbar. The Captain from a different perspective displaying his unique sky hook.”
You want to lock games up in the last seconds with that sky hook; it was not blockable.
What do we have here, oh… (reads Ruddle text)
“The big smile, and the point guard who invented and ran LAL Showtime.”
Magic. That’s Earvin Johnson.
(reads Ruddle text) “And then with no further introduction, the unstoppable and most ferocious Laker, the late great one, Kobe Bean Bryant.”
He was the assassin.
So it looks like you got a picture of you with all the statues.
I did. There’s one that’s not there that we walked right by, and I’m sorry I didn’t get it. But the voice of the LA Lakers for like 50-some years; he also had a statue. But it wasn’t – it was in action. He was at a desk with his big microphone, and he was calling the games.
Okay, and then we have this…
Oh, so now I see you’re at the AAE meeting here…. (reads Ruddle text)
“In short, we saw countless international colleagues. It was hard to move around as there was so many stop & chat friends to say hello to, far too many requests for picture taking, and countless young dentists who report they are watching TRS!”
And that’s a good thing.
And this is my favorite part here… (reads Ruddle text)
“Tens and tens of doctors commented specifically about you and how good you are becoming!!!”
You know, I actually –
Wait, let me finish… (reads Ruddle text)
“They expressed admiration and some international guys said your knowledge is amazing.”
And so tens and tens; I have to think that means like maybe 20.
It’s 19 and a half.
Okay.
No, there were a lot of them. And even on follow-up text messages from international friends, they not only said they are really enjoying the show, but they wanted to compliment you. They saw growth is what they said.
Okay, great. And then the last one… (reads Ruddle text)
“Gosh, after seeing so many faces from everywhere, I felt like it might feel like this in Heaven.”
Well where would you see so many people over the last 50 years in one place, except for maybe Heaven or Hell?
Well I really enjoyed this little text perspective of your trip to the AAE meeting. We did get a picture of Roberta Pileggi and her student, or her grad student and their thing. We showed that on our podcast, and we will talk more about your trip to the AAE meeting at some point, because there was a lot that happened there with the EndoActivator.
We will let this group on The Ruddle Show know about that good news at some point, right?
Right. Well, we have a good show today, so let’s get going on it.
SEGMENT 1: Endo History – 1968 Article “The Cracked Tooth Syndrome”
All right. So today we’re going to do another History of Endo segment. So those who know you well have undoubtedly heard you say before, everything old is new again. And you probably say a least once a week: create a future that is not about the past, but takes the past into account.
So the good news is you are not alone in that sentiment. It is echoed by greats like Confucious, Albert Einstein and Carl Sagan. When you study the past, it helps you to see patterns that might otherwise be invisible in the present, but ultimately giving you a better understanding of the present and where the future may be headed.
So you also enjoy history a lot, right?
I do love history. I love all kinds of history. Wars and societal conflicts, I like dental history, I like science history; yeah it’s really good. Because what I’ve always found out is if you want get a glimpse of the future, know the past. And so I think there’s a clue what history tells us, and it’s a clue to the present, the now, and then what we might be doing tomorrow.
Okay, so anyway. Examples of history that we really like is we’ve brought up in previous shows – which you’re a little bit behind and you need to get caught up; these are tens and tens of shows ago. We talked about Hydron back in the 70s, and then we talked about recently Resilon and how it made a toe-hold into the dental world. And then as mysteriously as they were ushered in, there were major problems and they were ushered out quickly. Our problem was we had respectable people, chairmen of departments of endodontics behind it. There was very, very – I will say bad research. And then I would say there was a lot of peer pressure, because you’re out there in the audience and reading this stuff, and you’re thinking these really important people said it, so maybe there’s something there. But that’s things we can learn about from history, and that might even prognosticate with the tricalcium silicate sealers.
And then I think if you think about our challenges today, they’re in some respects so different from our ancestors. But I think you would also be surprised how similar our challenges were then and now in terms of our ethics, our morality, and maybe even the ideas that we were going to do to fix these broken-down mouths. So I liked all that.
And then today, speaking of history, we’re going to go into an article from ’68, which is a long time ago. And the issue of ’68 is the same issue in 2024, same issue. It’s just a remarkable 56 years and we’re still having the issue.
So that’s what I think.
Okay, but the difference now; I think that there is a solution to the problem that’s maybe just on the very near horizon.
Unlike ’68, we’ve talked about it – and I’ll talk about it a little bit more in this segment – but we have something on the very near horizon now that will be very, very instrumental in changing how we look at this issue.
Okay, well that sounds hopeful. So what we’re going to talk about today is an article from 1968, and it’s called The Cracked Tooth Syndrome, and it’s written by Dr. Harold R. Stanley. This article was originally published in the Journal of the American Academy of Gold Foil Operators, and Dr. Stanley presented this paper at the ADA meeting in Washington, D.C., in 1967, a year before it was published.
And regarding Harold Stanley, he was an expert in oral pathology. And didn’t you see him speak before when you were a grad student?
Well we’re talking about history and looking back and getting off track if you’re Cliff. This is where we could take two hours. I really went into this. In fact, I made quite a few notes about just this one question. Because I wanted to see – instead of in pieces of the past, I want to now stand back in the sky box and look down the field and see all the moving pieces at once.
As I’ve said before, my mentor was Alvin Arlen Krakow, and he was chair at Harvard School of Dental Medicine. We were at the Forsyth Dental Center. But decades earlier, it was called the Forsyth Dental Infirmary. And that was a children’s hospital; it was one of the only ones in the country at that time. And Burke was a dentist, and he got accepted there, and he got his equivalent to what we call a degree in pediatric dentistry. He got a special recognition in his internship on children, and it led to – if Beth Damas is listening, she would want to know that this is how vital pulp therapy all started. I didn’t even appreciate that until I did this deep dive.
But I’m getting to the point. Because Harold Stanley did a lot of vital pulp therapy, Krakow didn’t really want him to teach it at Forsyth Dental Center where we were years and years later, because he wanted to have evidence. He wanted research, he wanted scholarly work.
So Burke went and met Stanley. And Stanley was at NIH in Bethesda, Maryland. And Stanley did all the histology on Harold Burke’s vital pulp therapy and those teeth; natural teeth. Those became slides that were given to each one of us graduate students, and if you watched Ruddle ever lecture and I showed you pulpal breakdown, that came from Harold Stanley.
Wow!
So Harold Stanley taught at Forsyth Dental Center; he taught at Harvard School of Dental Medicine. Just to be complete, he ended his career as an emeritus professor at Gainesville at the University of Florida Oral Medicine.
Well what was your overall impression of the article?
Well a fractured tooth, a cracked tooth, the Fractured Tooth Syndrome that he talked about, was exactly relevant to today. Because if you look at the forums, you look at the podcast, you listen, you’re out there. I’m out there. I kind of have my pulse on international endo. Cracked teeth are talked about all the time. Harold Stanley was just a little before his time. So anyway, that was interesting because it’s so current.
We’ve learned a lot more about cracked teeth through finite element analysis and through different studies. Earthman at the University of Irvine – you can go back and look at the shows, we’ve talked about him – but he’s part of this future we’re talking about for detecting cracks in teeth. And we learned a lot.
You know, in one year, you’ll get about one million significant loads on your teeth. So if you live to be 70, 80 years old – because you don’t really start chewing until you’re 10, so if you live to 80 – 70 years – you’re going to have 70 million significant loads on those teeth. Everybody think about stress fatigue. So that’s that.
And then I think just to say, maybe unlike 68 but similar, we’re living longer. But what might be different is we’re doing a lot more dentistry; more patients are seeing dentists, more exotic dentistry is being done. And the more we work on teeth – that’s the good news – but the bad new is we might just slow things down from a gallop to a trot.
Did you have an image you wanted to show us?
Maybe bring this up right now – thank you, I forgot. This could have been in the background. But as you can see when you look at – let’s go back two, just one before. I guess you showed that. But this was kind of back in Stanley’s era, and you can see. Look; you can see a very faint craze mark; overt stained fractures over the marginal – emanating out from alloys. Cracks between the alloys as the coefficient of expansion and contraction. So you see these in your patients every single day. Now you can go forward.
Just to clarify. The article mainly focuses on crown fractures.
Oh. Listen carefully; made a critical distinction. We are talking about incomplete coronal fractures. This is not subcrestal.
Okay.
So I think if you bring up these; I mean you can see – unlike what they had back in 68, there was no transillumination. You might have forgotten about that; that came out in 1970. So those of you who like a little bit of history, we got transillumination in 1970. But we know; we say you put it on a tooth, you play the light through, and we say a fracture line breaks a beam of light. And you can see a lit half and you can see a dark half.
This is more common in the middle. You see a lot of inlays; they could be amalgam, they could be composites, they could be gold. But people bite down, there’s plunger cusps from up above and they strike those inlays and they’re like splinters. And you can see fractures over the distal marginal ridge, down the axial wall, a little bit off to the mesial. And then of course nobody has any problem with that one. That’s just a lady getting pulled over because she’s leashed to a dog who jumps and startles the dog, and the dog jerks her off her feet and she does a face plant.
So that’s kind of a little potpourri of kinds of fractures.
Okay. Well let’s get to the article. The first part of the article discusses the difficulty in diagnosing a cracked tooth. And from what I understand, it can still be quite difficult today, even with the technology being a little bit different. Correct?
You know, when people come in with fractured teeth, Cracked Tooth Syndrome, it’s all over the place. I mean sometimes they’ll say – well first of all, it’s intermittent. Well if somebody tells you it’s intermittent, you think it’s going to hurt in the dental chair. It’s like the rattle in your car. You take the car in and you want to get it fixed, but it doesn’t rattle. So a lot of times they come in and they say every now and then when I’m eating and chewing, I’ll get like a sharp, lancing, transient pain.
So you start looking around, right? That’s what you do; you’re investigating. So it’s hard though, because you might not be able to make it happen. You can percuss teeth; percussion is not very good.
Yeah, they did note in the article that percussion seems to be somewhat ineffective in diagnosing a cracked tooth.
Right, and today though, we’ve learned from our past, these experiences. And we’ve learned to use – in the old days they started using like a burr loop wheel – it’s a hard, firm rubber. And you could not only bite down, but then you could rock around to simulate eating; work and balance, the mandible shifts back and forth.
You can do vital pulp tests, but these incomplete coronal fractures oftentimes are short of the pulp. So you’ll have pain from the dentin via the pulp, but you won’t necessarily be able to reproduce that.
So they could stain with dyes, they could do percussion, they could do the vital pulp tests which are typically cold and hot. And then you could take a radiograph, but radiographs rarely showed an incomplete fracture.
All right. So after Stanley talked about the difficulty in diagnosing a cracked tooth, he goes on to discuss the criteria that could make a crack more problematic over time. For instance, the proximity of the cracked tooth to the pulp chamber is key. And also the crack or fracture – having a crack or fracture considerably shortens the amount of time it takes for bacteria to reach the pulp. So maybe you could discuss this a little bit more.
Yeah. You know I’ll do the opposite. Caries. We always think of caries and it’s invading, it’s getting deeper, it’s progressing, it’s advancing, and it’s getting closer and closer to the pulp chamber. And so caries means it’s a microbial activity, and microbes secrete acids – acid phosphatase, etc. – and it eats away the dentin. But what’s the pulp doing?
The odontoblasts which line the periphery of the pulp, they’re laying down secondary dentin. They’re pulling away from the irritant. They’re getting smaller in their diameter. These canals are pulling away, they’re trying to; so it’s a slow, chronic process. So caries is slow and chronic and the pulp is always kind of working ahead trying to heal itself. In fact, I think we discovered that bacteria in about 90 days – I’ll just round it up; it was a little short of that – but 90 days in caries; Stanley showed that bacteria only move about a half a millimeter. So half a millimeter in 90 days. And then if you can keep the bacteria about half a millimeter away from the pulp, the pulp has a great chance to repair.
But the fracture – to your point – it’s an immediate invasion. It’s a highway. Whether it’s microscopic of not and you can see it or you can’t see it, it’s still a highway. And saliva is loaded with microbes and those microbes go right down that fracture and into open, patent tubules that are communicating directly with the pulp proper.
Okay. When you were reading the article, was there anything that struck you as very different than how we think today, or maybe just seemed a little bit odd?
You know, I made a comment over here somewhere – I don’t know where it is but it doesn’t matter. There’s two types of pain. But I want to make sure you understand. The two kinds of pain are from the pulp. But there’s different nerves, and the myelinated C-Delta fibers are the cold response; the sharp, immediate zingers like electricity. But your unmyelinated fibers, they’re very slow, they’re much slower in action, and that’s the heat. So heat means the pulp is probably becoming necrotic, there’s microbial organisms in the pulp, they secrete gasses, gasses expand when there’s heat and pressure on the tooth, and so you can get pain that way.
Okay, because Stanley talks about in the article the difference between dentinal pain and pulpal pain; and that’s kind of what you’re referring to now.
Yeah. In fact I told you I disagreed, and I didn’t understand until last night and another night. I was re-reading it again and I started to get into his head. So he’s talking about the dentinal pain. That would be like your delta fibers – the myelinated fibers firing off, and you’ll get the quick zingers. But he’s saying that if you start to hear them say it’s hurting to heat a little bit, then he’s thinking that’s an irreversible; that’s more of a pulpal pain versus a dentinal pain. So it has to do with these fibers.
Okay. So if you’re getting your teeth cleaned at the dentist and you feel a little zing, that might the dentinal pain but not pulpal pain?
Yup. So I want to make sure the room heard this correctly. The myelinated A-Delta fibers, cold; that’s like a dentinal thing in the dentine, but the dentine communicates it to the pulp. Whereas your unmyelinated C-fibers; that’s the one that’s going to be the heat and the necrotic pulp.
All right. So he then concludes the article talking about some recommendations to both facilitate diagnosis and managing the cracked tooth. So what are the 1968 recommendations, and is that still what we do now? Or do we do anything different?
Well, I mentioned this just a little bit ago, but in 68 they had dye: Methylene Blue, Chinese Red. And the idea was you would flood it into the tooth and then flush it off, and then maybe the dye would absorb into a thin fissure, like a crack. They also said that wasn’t so useful for the very early ones. So sometimes they would impregnate Methylene Blue into a provisional temporary, and have you go home and chew and eat and work, and then take it out a few days later; because maybe the dye had time – with the tooth moving on a micron level, the segments moving – you would probably get the dye more thoroughly introduced into the fissure so you can see it.
So they did that. They probed the sulcuses, because we all know if cracks get too deep – but we’re talking today, remember, coronal incomplete fractures. But if you get subcrestal and you start to see pockets and probes will be helpful. They checked the occlusion; we did that. They used marking paper to make sure you’re not beating on a tooth too hard, or if you are, relieve the opposing tooth or even the one in question. Check for restorations that could be defective and they might be leaking. And of course they had the bite test. And we’ve talked about the Q-stick; take a stick with a little cotton on it, then you have them bite down, rock around that. We have the tooth sleuth, there’s different things that I think are pretty much old school.
The new school; the new school is exciting. I just mentioned; they didn’t have transillumination when they wrote this paper. Can you imagine? That second slide we showed just a little bit ago; you can go back to that second slide. Can you imagine putting a bright light behind this tooth? I mean I think you’re going to talk to your patients different. I think you’re going to talk about maybe an onlay, cuspal protection, maybe a crown. Because that is a tooth that might be totally asymptomatic, but it’s an accident ready to happen.
And then of course we have CBCT. We take X-rays three angles, but if you do tomosynthesis, you shoot one time but the way the ports are angled you get seven views. So you can go through a stack and you can see different angulations of the same tooth. And the CBCT is quite helpful.
So then we have Innerview, and that’s coming. We’ve talked about it on several shows, including having Dr. Cherilyn Sheets on, and she’s brought us up to speed. Do you want me to tell a little bit about that? That’s later. We’ll talk about that a little bit later.
Well we’ll talk about that in just a second, because that is the solution that’s just around the corner. This cracked tooth thing has been around and diagnosis is a problem; there’s a problem with diagnosing it. It’s been around for decades and obviously claimed many victims; whether it be people who just experience a lot of pain while they’re chewing, or people who pay huge amounts of money to restore structurally unsound teeth that have cracks.
So you said Innerview is coming, and so now go on. That’s pretty exciting.
So the new things are transillumination, CBCT, microscopes didn’t exist back then – I’d better throw that in or I’ll get shot – and then the Innerview. The Innerview is an electromagnetically driven hammer, taps on the tooth.
Percussion.
They’ll actually see it later in the show.
Actually, well I think we – we’ll we’ve talked about it a lot on the show already.
But they’re going to see it later on another segment I’m doing later. But this percussion sends to the cloud – because there’s a chip in the hammer that hits the tooth – sends to the cloud. It hits the tooth; the tooth oscillates. But the tooth’s oscillation now begins to dampen back to zero. It is doing an energy return graph in real time, sending you back a curve of that tooth. So if we have a nice, bell-shaped curve, the tooth is fine; a round of applause. But if you start to get double peaks, or you see this and then a spike off like that, you’re dealing with a cracked tooth.
So we have a method coming with Innerview – that’s Perimetrics if you want to Google it – and you’ll find absolutely a game-changing thing and cracked tooth diagnostics; not only coronal, but radicular. And the news gets better. It will even distinguish between a loose filling and a coronally cracked tooth.
Yeah. I just thought it was fascinating how in the article it was really emphasized that percussion is not effective in diagnosing a cracked tooth. And then here Innerview is using percussion. Because it can understand the feedback that it’s getting. It’s so sensitive – the AI is so sensitive, that it can understand the feedback that it’s getting from the percussion and recognize that there is a crack, and to some extent even categorize what kind of crack it is.
So I just think that whereas the patient and the clinician couldn’t really interpret the feedback from the percussion, AI can. And without causing the patient any pain.
I mean think about it. (tap, tap, tap) When you do that, you only know yes or no. It hurts/it doesn’t hurt. But the little hammer is looking at a database of millions of tests. And so machine learning is diagnosing where the crack is, the extent of the crack, how the crack propagates and runs. That’s the difference between percussion in the new era with technology, versus Cliff taking a mirror like we all like to do and hit the tooth.
So there needs to maybe be a new article called The Cracked Tooth Solution.
Well that’s coming.
Do you have any final comments, or perhaps you’d like to crack a joke?
Well you know, a cracked tooth is usually when a piece separates, it’s concerning, it’s painful, it’s something that needs immediate attention usually. And that means an office visit. So it can be kind of an anxiety type thing, and I think we’re had a show that needs to end on a very positive note.
So I hope the international people get this joke. I never told jokes overseas; they say just blow it off. But I’m going to try it because I’m in Santa Barbara; that’s the difference.
So why do Buddhists refuse Novocain when they have their cracked teeth repaired?
Why?
They want to transcend dental medication.
Okay, that’s pretty funny. I know you had actually quite a few.
I have six of them.
Okay, give us one more.
Oh come on; I don’t want to make you crack a smile.
Okay, all right. Well thank you for the information and we hope you enjoyed this segment.
SEGMENT 2: Management of “Through & Through” Resorptions
It’s absolutely great to be with you again. I’m kind of getting into this thing; the family’s talking about the Road to 100, so this is #94 and here we go.
I’ve talked about many different topics at different times, and I hope today will be very useful for you. We can talk a lot about resorptions and we can talk about their etiology; we can talk about internal. You can see internal. Simply, we understand it’s a pulpal problem. If we remove the pulp, the dentinoplasty (inaudible) activity is arrested and we can preserve the tooth, assuming it’s not too badly damaged.
So we’ve already talked about internal resorptions. We have external resorptions that are almost always related to trauma. It could be trauma from a car accident; it could be orthodontic. In other words, controlled trauma. So you could have controlled tooth movement that leads to external resorptions.
Today I’m going to focus more or less on through and through. The ones that are internal and then they can eat their way out; or it’s outside/in. So it can be inside/out or outside/in. And that’s kind of the topics I want to talk about today. And we’ll do the big eraser in the sky. So here we go.
So somebody comes into your office, and you see this X-ray. And they have just finished orthodontics and it’s a little bit sad. The parents are not happy. Especially when you start to show them the X-rays and what all this implies. And if you raise a flap on this case – and I’m not going to show all these cases start to finish; that’s why you joined the continuum, to get the deep dive if you will. These are quick, fast-moving; I’m supposed to be 20 minutes, maybe 25. It’s just to whet your appetite for something even more. But when you see that film on a young patient, there’s a lot to be considered. And you must be talking to the parents as well. And if you bring a flap up and you elevate it, you can begin to see; this is, in fact, inside/out. You can clean all this out, but we can probe and go right into the pulp. So on another time and another case, we’ll go back to the Andreas and Trauma series, and we’ll talk about more traumatic injuries.
So that’s one kind of a case. And you can see then how important it is to be monitoring your patients during orthodontic tooth movement; or after any kind of trauma. Because a lot of times these are very silent; they don’t hurt. And by the time the patient will tell you something’s not quite right, gums are a little tender, I have some bleeding around the crown of the tooth; oftentimes you get something that looks pretty serious.
This one is another one that comes in; this is a bridge abutment. This is a very strategic tooth in the most funereal sense. It’s holding a bridge, and you can see this tooth is absolutely moth-eaten. And there was a lot of arm twisting by everybody – because I usually work with interdisciplinary treatment, so there’s the general dentist, there might be a periodontist, there could be an oral surgeon. There could be a lot of different people involved, and everybody was pulling for Ruddle to try to do something. Was there anything I could do?
In today’s world – this was about 35 years ago – in today’s world, I think I could have pulled it off. You think oh, come on! Nobody can pull that off. I’ll show you in future segments. If you just keep coming back, we’ll show some pretty remarkable stuff that anybody can learn to do.
But let’s see how that might look with the flap up. So it’s not easy to raise the palatal flap, you know that, and when you get in there, you might think there’s blood everywhere. Well there is unless the pulp’s already necrotic. So we talked about that Stanley paper earlier in this very series, today’s lecture, and we talked about John Stanley in 68, we talked about fractures confined to the coronal part of the tooth, incomplete. But when you start to look in the mouth mirror, when you have that little mouth mirror, and you realize that like Stanley said; if the egress is in the pulp and it gets chronic, the pulp’s going south and they can become necrotic. So they’re not always a big vascular issue. Oftentimes they bleed copiously.
So when I looked in this mirror shot – and there’s just nothing from about right here to right here, and I haven’t even shown you up in through here yet. So anyway, that is not a good prognosis and there is not very much left. And then when you think about this bridge, the whole thing is in question.
So I showed you a couple slides just to get going, because what that really said was – in a nutshell – please follow your patients. Take the periodic films more frequently if there’s been a history or an episode of trauma so that you can catch these things early versus late.
All right. So what’s some of the things we can do? It’s the usual tricks. Remember Stanley talked about what they did in his day? Well, they had radiographs back then, but I would just add please, three angles. Come from the distal, straight on, move the cone, come from the mesial. The cone can move about 30° so you can really start to get more of a 3-dimensional interpretation of a 2-dimentional object.
Tomosynthesis – we’ve had Tyndall and different people talk about it – but it has seven ports. So one click and you’re going to get a stack of seven images. So you’re going to get different angles with just one shot. That would be something that they didn’t have in 68, of course; it has just been recent. Portray is the company.
CBCT came to the United States in 2001. It was a little bit earlier in Europe, but really it’s a pretty new technology; it’s less than 25 years. But this is a game-changer for getting the coronal, the sagittal and the axial slices. And you're very, very good – those of you that have it – at interpreting that information and treatment planning using that information.
Well there’s something else to be talked about, and we talked about it earlier. We talked about this. Innerview. We talked about it in terms of the fractured tooth. But if you have through and through defects of resorption, you’re going to have a loss of the PDL. So when that little hammer, electromagnetically driven hammer, lightly taps the tooth five times, you’re sending up into the cloud a record of the oscillation of that tooth, and then it starts to dampen and ceases to move. You’ll get an energy return graph, an ERG. And that is not only wonderful news for the fractured tooth dilemma that we’ve talked about; but if you think about cracked teeth, they often have PDL extensions. And that means that any loss of periodontal ligament or surrounding bone, it’s going to give you a different energy return graph.
So those are some of the things that we can add to what Stanley talked about a long time ago. And you can go back to Season 2, Episode (8), and that was just one time we talked about it, but we’ve talked about it several times.
This is the usual pulpal sensibility testing. You can do your cold test, the hot test. The only thing I’ll say is I’m not ever doing both. There’s a refractive period after a cold test where any other subsequent test would be probably inaccurate; you might even get a false positive. So the patient is now going to fool you and you might start a whole treatment plan that’s not necessary.
So if the patient says it’s hurting to cold, I’m running a cold test. If they say it hurts to hot, I’m running the hot test. If they say it doesn’t hurt to hot or cold, I’m running the cold test because it’s easier. So we have the hot, the cold, and then we’re probing every sulcus.
Now in the Stanley lecture, we talked about coronal fractures. You’re probably not going to have a PDL or pocket problem in a deep, narrow defect. But, with talking about through and through resorptions, depending on the destruction and the amount of time, then we might have to have a probe. And if you have to use a little bit of anesthesia to put up into that vestibule or right around the mucosa there, do it so you can probe with intentionality. Sometimes we say there’s no pocket, but there is a pseudo pocket and when there’s anesthesia, yes, there is in fact a pocket.
So bread and butter stuff; you know how to do it. We’ve talked about it on all the shows. Different shows talked about each one of these. So if you want to get a little bit more information on that, you can go back.
But carrying right along, we’ll look at the first case of the day. The etiology was trauma, and I just want to show you in this one slide – I guess I could spend 20 minutes. The family would go crazy, I’ll tell you. Look at the central incisor; it’s a block of dentin. So this is a physician. One tooth calcified and completely mineralized; and when I say “completely,” who’s to say if you cut an access and we’ve talked about different tracking methods like X-Nav. You might be able to get through there, if you had to, if there was in fact a lesion of endodontic origin; a LEO.
Contrary to this, you see we’ve lost a little bit of the incisal edge. There’s a chip. There’s a little chip there, you can see loss. Look carefully. I won’t go over it so you can see it. It’s faint; it’s faint. It’s a little hairline crack. Stanley would say that’s a highway to Hell. That’s a highway of saliva and microbes, rushing through dentinal tubules along the fracture sign right into the pulp proper. It happened and over chronicity the tooth became completely necrotic.
What else do we notice? Beth Damas would like this because she talked about root end closure. Nobody did any dentistry, but do you notice there is apparently a dentinal bridge. We talked about Burke earlier in this lecture; he was the maestro of calcium hydroxide pulp incorporation. It was calcium hydroxide in a methylcellulose solution. So we have used that for decades, haven’t we? For pulp caps, for pulpotomies. Gave away a little bit to MTA and some of the tricalcium silicate sealers and those kind of repair materials.
But you can see calcification. This tooth is almost like it was an adolescent tooth, the chamber is so big. And this probably was originally a lateral canal I’m thinking. But that lateral canal has undergone resorption and it’s a blowout. And look where the lesion is. Look where the lesion is. The lesion is what we call asymmetrical and it’s on the lateral aspect. And the lesions form adjacent to the POEs, portals of exit.
I’m having fun. So how do you clean that? Are you trying to get a nice shape going; are you trying to remove more restrictive dentin? You don’t have any restrictive dentin; it’s a highway all the way up. And you have maybe a little bridge. So the only way you’re going to really be able to do this cleaning is not with files and not with long, old-fashioned (it never really was done) soak periods. People talked about soaking with sodium hypochlorite and doing something else in another room. But you need like a laser; you need something like GentleWave. Those are going to be technologies that are tens and tens of thousands of dollars.
But for $1500 we’ve talked about the new SmartLite Pro EndoActivator, with a polymer tip that can slap around in there; mechanically it’s cleaned by slapping the walls. It also generates fractures in the liquid, the liquid fracture interface. Bubbles form, bubbles are unstable because of heat and pressure; bubbles expand, they implode, and they send out shock waves. And that’s how we clean off the instrumented portion of the canal. So there’s the instrumentable portion and the non-instrumentable portion, and we’re going to need something other than files to clean into the lateral deep anatomy.
So this is a way. You can see there’s been some significant things. I want to repeat this again. We’re probably running just a smidge over, but just recently a few weeks ago at the AAE meeting, head-to-head GentleWave was compared with the SmartLite Pro EndoActivator. And the SmartLite Pro Activator was more effective at removing e faecalis, 91 compared to 89. It wasn’t statistically significant, but what is statistically significant; one is about 90-100 thousand, GentleWave, and we’re talking about $1500 technology. And it did better in Pileggi’s wonderful study. And I want acknowledge Addison Valdes, Gina. Gina is very, very smart; she’s one of the futures of endodontics. She’s one of the big futures.
So back to the case at hand. You’re going to make your access, you’re going to do so much shaping. It’s a necrotic tooth so it’s not so difficult. You're not fighting collagenous, bloody, inflamed tissue. Listen: customized cones. You can squirt these cases sometimes, like with an obturator or a calamus or something like that. You can squirt them.
But you can also sometimes fit cones. Sometimes you have to fit a cone butt end first. Sometimes we cold roll those cones, to change their tapers. Sometimes we use heat on glass slabs and roll them to get the desired shape. That’s a customized cone. Now you have a customized cone that’s not binding laterally; we want it to bind in the apical third. And once we have that going, we can downpack; we can move thermal softened filler materials into difficult areas; small areas, big areas, blowout areas. You might mix your cement a little heavier; recognizing you’re looking for a huge splash, maybe a massive splash. But in this case I was pretty happy. We provisionalized the tooth as we did in that era, back in the general dentist. And of course, because we saw this little hairline crack in here; because we saw that little thin crack. I think you can see it; camera’s pushed in as much as he can. He being the shooter; Isaac Kirschner.
All right. Follow the cases over time. Keep following the cases. Because resorptions can sometimes revisit and you want to make sure they’re checkmated. But if you can remove the etiology – this time it looked like it was internal/out – so I think if you can get the pulp out of there, get all of the breakdown parts out of there and disinfect properly, it’s inevitable. The endodontics is a reparative and regenerative material and a procedure.
All right, let’s go again. This was sent in to me and the chief complaint was severe pain to cold. Well usually teeth that have had previous endodontics do not respond to cold; even when it appears like there’s deficiencies. So I see a PDL up here; I see maybe a little bulge, and you see a gutta-percha cone ending about right in here. So they did sort of a good job. This is kind of like – you’ll find out in a few minutes when I talk about the journey of 1000 seconds and you’ll tie it back to this case. But that wasn’t done very well. That case you can hammer on it, it can break sticks, it doesn’t hurt; you can put cold all over that tooth – doesn’t hurt. Cold provoked a massive stimulus.
So this tooth lingered; the cold pain was sharp, immediate and lingering. And you’re thinking, it’s pretty calcified; I wonder why there was sufficient tissue there to even respond to the stimulus of cold? It didn’t.
So I didn’t really see it. You’re not really seeing it, are you? You look at this bone and you see the little trabecular white lines; you see narrow spaces, and you kind of maybe see something in here. But it’s about the same. The canvas is about the same left to right. Yeah? I hear you. You're all going yeah; it looks about the same, Ruddle.
Well, we went in there and did two-visit endodontics. Lots of bleeding; blood was pouring out of the palatal canal virtually the whole time I was instrumenting. Calcium hydroxide into the bloody canal. Bye-bye, they were provisionalized. Have them back in a week or two or whenever your schedule allows. And the bleeding was arrested; we flushed out the calcium hydroxide and I packed it.
I also want to talk about the powers of angles. The powers of angles. This is a wildly distal view if you’re looking in terms of the reference of the first molar. But if you’re looking in terms of the reference of this tooth, it’s about a straight-on angle. I’m pretty close and there’s a lot of glare for me, but I kind of see the palatal there. I kind of see the MB coming around like this, and I see a DB over here like this. So I’m just coming right on; I’ve got an MB on one side of the palatal, a DB on the other side, and the palatal is in the middle. So straight-on angle, but it’s not straight-on relative to the first molar. You know those things, but those are tricks that your assistants learn to do. So when you’re reviewing films thoughtfully and carefully, you’re getting multiple different looks at the same tooth.
So back to the pack. That was kind of a big surprise to me. I called the patient that night and she said doesn’t hurt at all. I said can you bite on the tooth; she says yeah, and it feels terrific. And I said how about the cold – knowing for sure the cold was gone. She said first time in months I haven’t had severe pain to cold.
So by keeping – the dentist kept her in the office too long, the cold was reported many, many times over months and months and months, and finally when the patient was getting a little frustrated, I caught the consultation and it led to this.
Now let’s look – so there’s no sealer coming off the MB; you can see an MB1 and 2 coming around the portals of exit, two little puffs. You can see the DB in this view. It’s not coming off the DB; you can see a sharp delineation between GP sealer interface with dentin, a little bifidity apically, a little bifidity apically, different views, they look at little different. But now, because we saw the MB was clean, the DB is clean, we know for sure it’s off the palatal. Of course that matches the clinician’s expectations because of all the blood pouring out of the palatal root during the entire first session.
So how long will it last? Ask my staff. It was actually my wife, Phyllis. She said do you have a recall? And I said no, I don’t have a recall. This is rare. Ruddle almost always gets recalls. This patient I think moved was what happened. But I knew for five years she had the tooth. So no. Who knows how long it’ll last? But remember; you’re trying to slow disease down from a gallop to a trot. If you can keep something there for 10 years, what would the profession look like in 10 years? What would we have to work with that we don’t have today? We might even have a better prognosis then.
I’ll go quickly; we have another one. You might say get it out Cliff; haven’t you heard of implants? We give the patients every opportunity to have implants; if they want them they can have them. I don’t do them. But a lot of patients go well take a shot at it. So it’s just time and money. So if some people don’t want you to gamble with it, well fine. Get it out and do something else; a bridge or do a restorative implant; maybe two.
In this case though, it’s a miss. There’s been previous treatment, massive lesion, almost no bone on the whole distal. It’s draining like crazy, and it’s been draining for months and months. So you’re even thinking there could be calculus and microbes and stuff on the root; even if he gets a good result endodontically, there could still be microorganisms on the external root. So what we did is roll up our sleeves and went to work.
I had to go borrow this file from Sears & Roebuck – that’s a department store over here in the United States, and that’s where you get screwdrivers and sheetrock and hammers, chisels and stuff like that – so that’s something off the shelf of a store like that. Because nothing in dentistry fits that canal; that canal is huge. Notice my files – a floater; it’s a floater.
But that’s about where it dries, so we’re going to work to the drying point; that must be the portal of exit, that’s the thinking. I’ve talked to you already a little bit about making cones, custom cones. Here are two side by side custom cones that are heat softened, out of the mouth, and brought in and cast; doing this several times and repeatedly until my cones kind of look rough and I can see striations and scratches, and they’re pretty much taking an impression of the intaglio of the distal – the DB and the DL – that are massively resorbed. And look at how short the roots are.
So boom; you pack it. And you’re going to say Ruddle, you over filled the distal. I don’t call that over filled. Do you call that over filled? I call that surplus after filling. And if we read the Schilder work and go back decades ago, like we did with Stanley earlier, we can learn so much from the past. But we know that gutta-percha and the sealers we use are biocompatible. We know – and I have my own research from when I was at Harvard Forsyth Dental Center – we did work on prisoners; we showed osteoid, precursor bone scaffolding going right through sealer, butting up the side of the root. So the healing for me was inevitable, if I got a seal. And apparently I did get a seal, because some years later – this is about a 10 year later recall – new crown, great osseous healing. You started from something that looked like a disaster, and it’s quite thrilling. And you learned a lot about you and your patients learned that you are a good person if they have a tooth problem and they want to retain – they want retention of the tooth.
All right, we’ll quickly move to surgery. We only have two cases left. You know, when you do these things, they’re fast, they’re staccato like a Gatling gun. It’s to get you interested. You have cases like this too, to show you little glimpses of how to do it. But if you want to drill down to the continuums and go step by step by step, and have that apply to a myriad of situations, that would be a plus.
So Beth Damas would have liked this; I keep talking about Beth. If you don’t know who I’m talking about, go back and look at a previous show. She talked about vital pulp therapy and how to use the patient’s own pulp to induce Hertwig’s epithelial root sheath to elaborate dentin to get re-enclosure. Well nobody know about that apparently with this case; I’m about the third or fourth cowboy inside the tooth. This is my pre-op. They’ve had endodontist #1, endodontist #2, okay. But the roots have reverse apical architecture. They’re actually like a funnel; they’re going the wrong way, so what am I going to do?
So what I did – there’s lots of things. I could have used a barrier – I want you to hear the words – I could have used a barrier and packed it against the barrier. The barrier gives us a backstop to pack against and gives us hemostasis. But in this case I decided to clean this out the best I could – you can see the sinus track, fistula, and that’s Ruddle’s pack. Now that is what I would call, clearly, surplus after filling.
Oh the language. It’s always about the semantics, isn’t it? For you, it’s an over fill; for me it’s surplus. I did think in this case – today I would have left it. Today I wouldn’t have flapped it. So I flapped it, because I thought well, this is going to go back and it’ll circle around the world, and everybody will say it failed because Ruddle put 10 yards of GP out through the lateral and apical portals of exit which are so badly resorbed. I mean this is bigger than 160 – that’s the biggest file they make – that’s like about three 160s.
So we went in, used super EBA in that era. And I corked it here; you can see it in here like this. Here I just took a scalpel and trimmed off the surplus, and just left it gutta-percha. And you can see many years later; the patient’s had the tooth restored and that tooth is an integral member of the anterior arch. So saving teeth one tooth at a time.
And the last case is a guy 89-years old – he was a dentist – and he came in with a cane and he was quite feeble. And I saw these films and I just said geez, you’ve got a big problem here. He knew he had a problem. He said people told me 10 years ago I had a problem. I said well why didn’t you fix it; you're a dentist? He said well, I didn’t think anybody could do it. I said good; so you waited 10 years because it could get a lot better, right? So now you’re seeing me.
So you notice everything’s good, but we have the first bicuspid; we have a canine. You can see massive, massive blowout through and through. You can see over here it probes a little bit. It’s an inside/out, it’s towards us so it looks like you have a little wall of tooth. You think you have some tooth structure, but remember; if you had your CBCT or you took multiple views, if you probed, if you did the things we talked about earlier in this very segment, you would know that’s through and through. How about palpation? It was sore; blood came out.
So that’s what I said. If you want to save them, old-timer, maybe you’re in right office but with the wrong teeth. So he gave me – he was a very gruff guy, he said go ahead. So I went ahead and I did the root canal.
On this one, you're going to need to understand; I’m using MTA. And on this one, I’m fitting the cone; I’m fitting a master gutta-percha cone. And then I’m going to use vertical and pack down. And then I’m going to lay a flap, and then I’m going to clean up, and that’s what I’m going to do. So here we go.
These are intense procedures, because these older people don’t tolerate a long procedure. This is the second – or I’m sorry – this is the first. And I packed it; you can see the gutta-percha in through here. You can see some curved pulp canal sealer here. We have an intact wall, that’s beautiful; I have tooth structure in here, let me clear that out so you can see it. So I was very lucky; it didn’t go around and get into interproximal areas. So I have it carved out, I can see my gutta-percha, and we pack it and we seal it.
This one was just straight MTA, so MTA the whole way. I used ultrasonics, indirect ultrasonics. So you put the tip in – the ultrasonic tip of that era did not have the plastic polymer EndoActivator – and then put ultrasonics on the shaft and vibrate that file. And just like you vibrate mud – concrete – to go into a form and get a good surface – no voids. Just like you vibrate dental stone into an impression model, we vibrated mud into this tooth. And you can see we have really quite a remarkable adaptation with no surgery. This is part of the ledge here from it. But here’s one that we repaired. And it had bifidity, we got good hydraulics. And then the one in the other, there was no bone loss; there was nothing that would worry me about flapping that and carving out all that bone to free that up. So that’s kind of how that ended.
So what I’d like to say in closing. We’ve talked about five cases; we’ve talked about three done conventionally and two done surgically. But we can do a lot in today’s world with endodontics if we have a few ideas.
CLOSE: Demotivators
All right, so it’s been a while since we’ve done demotivators, so we’re going to close our show with some demotivators. And if you don’t know what these are; these are some cards that I gave my dad a long time ago. And they have kind of a nice, inspirational picture on the front, and then a word that can mean a lot of things, but then it adds a little saying. It’s kind of a little bit sarcastic, sometimes it's a little bit ironic, kind of humorous, but maybe it still teaches a lesson.
So anyway, we’re going to do some of these today.
Yeah, be glad I haven’t mailed you one.
Okay. So the first one I have is Retirement; and it shows a pencil that’s all the way worn down. And it says, because you’ve given so much of yourself to the company that you don’t have anything left we can use.
Well, you’ve worked hard your whole life; you’ve given so much to so many for so long. You’ve created a legacy practice. But you know, decades have gone by and for whatever reason, health-wise or it’s time, you need to retire. And when you retire, you are no longer of any use to your patients. Your patients don’t need you; you have nothing left to give.
I guess that would be kind of a downer, so we’ll end on when you retire and your pencil was short from the practice career, get a pencil and start a new chapter.
Yeah, you just said a word that I heard: Legacy.
Oh!
It’s an ongoing theme in our Season 11, Road to 100. And you know, I think that the idea of retiring might mean that maybe you’re just cutting your legacy off right there. But you want to keep going, right?
Sharpen the pencil and start again.
Keep working on your legacy. Even after you retire from one job, maybe you still work on it your whole life.
Yeah, why not?
Okay, next card. Ambition. And it shows a grizzly bear about to eat a fish. Well maybe it’s a grizzly bear; it’s a bear. Okay, it says ambition: the journey of a thousand miles sometimes ends very, very badly.
Okay, so you do occasional endodontics. Not so often, but you love it. You have a huge ambition to do endodontics; you are inspired to get to length. You’re treating an abscessed tooth, the tooth is elevated in the socket, there’s a frank lesion apically, it’s a molar. And you go well, I have a great desire to get to length and I’m going to open this tooth up. And you start working those files, and 1000 seconds later on the journey – which is about 16.7 minutes – you have blocked the canal. Worse; it is ledged and perforated. It didn’t end well.
So maybe your journey on that 1000 seconds to length needs to be reassessed.
Okay. Well when I look at this card, I think of legacy. And I’m thinking that you’re ambitious to create a legacy and really stand out from everybody else. And I think this fish was trying to stand out and then look what happened; it got eaten.
Well the legacy of the salmon is to go upstream and lay their eggs, and then that’s it. Right?
Right. So maybe just be cautious with your ambition.
There you go.
All right. The last one is priorities, and it shows these funny statues. And it says hundreds of years from now it will not matter what my bank account was, the sort of house I lived in or the kind of car I drove. But the world may be different because I did something so bafflingly crazy that my ruins become a tourist attraction.
Okay. So I’m thinking, I have some notes here. So you make a lot of money, you buy a nice car, you always – the bucket list car you always wanted – you get the great house. But in a hundred years, they’re all material things and they are gone. I might add, for those of us who are alive; we’ll also be gone.
So what’s the clarion cry? Maybe do something crazy; something incredibly cutting and wonderful with your work that is within those patients that you see daily. And maybe it’ll serve as an inspiration to future generations of dentists.
Okay. Well when I look at this one, I definitely think of legacy.
Well it is a legacy.
Because you’re creating something that will be around long after you’re gone. And I also think of the statutes in front of Crypto.com Arena that you were seeing.
Very good.
And so that’s a little different kind of statue than this one.
Was there a Stanley statue? I didn’t notice.
I think we need to make you a statue.
Well not me, but I mean out there there’s the great ones; we’ve got to get a Center to cluster these brazen, brass, wonderful, futuristic things.
Right. So you want to do something that will be around long after you’re gone? And if you can’t think of something really game-changing to do, maybe you just make a statue of yourself. So any final words?
No. I think if we’re talking about these three demotivators, there’s always a flipside. So always be thinking about things. There’s always an ending and so there’s always a new beginning.
Okay. Well thank you; we had a great show today and we’ll see you next time on The Ruddle Show.