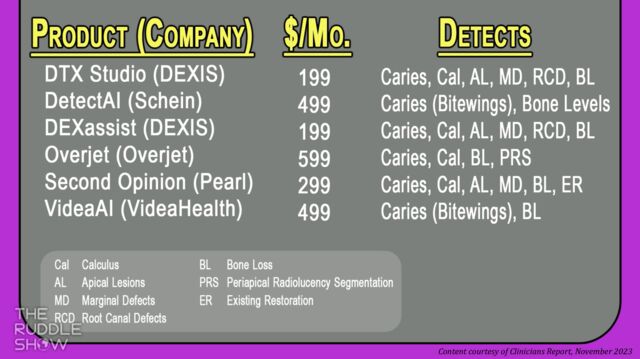
Featured Graphic from The Ruddle Show: Knowing the Difference - AI Diagnostic Software Packages (content courtesy of Clinicians Report, November 2023)
Artificial Intelligence & Disassembly Differentiating Between AI Systems & Paste Removal
The show begins with sharing some Dentistry Fun Facts… Let’s see if there’s one that even surprises Ruddle. Then, do you feel pressure to jump on the AI bandwagon, but have no idea where to start? Well, Ruddle and Lisette explain what AI diagnostic software packages are available, how they differ, and that feeling hesitant to purchase one is very much OK. Next, Ruddle is back at the Board focusing on the removal of the more traditional paste fillers. The episode concludes with a bit of humor at history’s expense; Ruddle and Lisette share a couple vintage dental ads.
Show Content & Timecodes
00:16 - INTRO: Dentistry Fun Facts 06:09 - SEGMENT 1: Knowing the Difference – AI Diagnostic Software Packages 25:18 - SEGMENT 2: Removal of Traditional Paste Fillers 54:30 - CLOSE: Vintage Dental AdsExtra content referenced within show:
Other ‘Ruddle Show’ episodes/podcasts referenced within show:
Downloadable PDFs & Related Materials
There has been massive growth in endodontic treatment in recent years. This increase in clinical activity can be attributable to better-trained dentists and specialists alike. Necessary for this unfolding story is the general public's growing selection for root canal treatment...
In a previous interview, Endodontic Therapy and Dr. Cliff Ruddle discuss nonsurgical retreatment and the integration of traditional and modern techniques for achieving excellence and producing predictable outcomes...
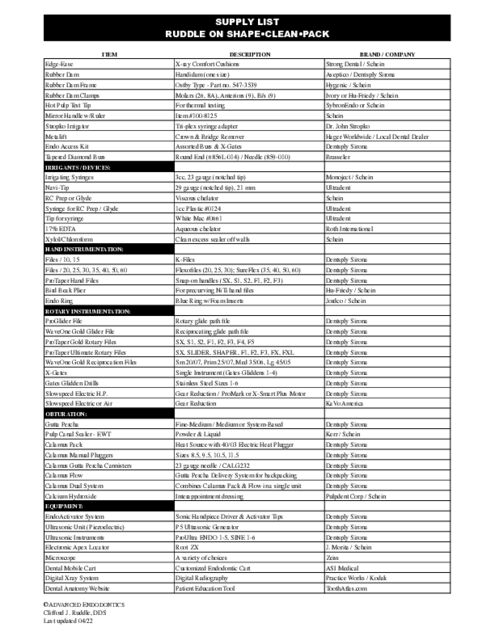
Ruddle on Shape•Clean•Pack Supply List and Supplier Contact Information Listing
Ruddle on Retreatment Supply List and Supplier Contact Information Listing
This transcript is made available by The Ruddle Show in an effort to share opinions and information, and as an added service. Since all show text has been transcribed by a third party, grammatical errors and/or misspellings may occur. As such, we encourage you to listen/watch the show whenever possible and use the transcript for your own general, personal information. Any reproduction of show content (visual, audio or written) is strictly forbidden.
INTRO: Dentistry Fun Facts
Welcome to The Ruddle Show. I'm Lisette and this is my dad, Cliff Ruddle.
How are you doing today?
Good. How about you?
Excellent. And I hope our audience is really excited about the show.
Okay. We thought we would start off today with some dental fun facts because, well, they're fun. So, fun facts can arouse curiosity, they can be unexpected and catch you off guard and you might even learn something.
Yeah.
And believe it or not, they even have the potential to raise new questions, cause you to think critically and maybe even change your perspective. This actually just happened to us when we were talking about these fun facts before this segment started.
You weren't referring to me, were you?
We had a little math lesson.
Yeah.
Okay. So, looking at this list of fun facts we have, they're just kind of general ones about dentistry, with were there any that really kind of struck you?
Well, yeah when you do the math wrong it really did strike me. So, the fun fact was did you know that in North—well, no, the United States alone, we consume 14 million gallons of toothpaste per year. And I thought--yesterday I thought, come on, that's a lot, isn't it? And I didn't understand the importance of the dividend and the denominator and I got them flipped up and I had a staggering number. So, I was going to tell you it really surprised me. But if you do the math correctly, it's about a half a cup per person per year.
Which is very different than 25 gallons per person a year.
Well, I thought they were bathing in it, cooking in it, wiping their car down, you know, like a little brace, even the paint just shined. I didn't know. Thank you for the correction on the math.
Are there any others that kind of struck you as surprising?
Well, I think as dentists, we mostly know this is a consumer thing you found, so it would be very interesting for consumers, but yeah, I think when we look in people's mouths every day we should realize that 90% of all systemic diseases have oral manifestations. I think the colleagues know that, but for instance there’s cancers, cardiovascular disease and diabetes/diabetics come to mind immediately.
See I think that's pretty interesting that it's 90% have oral manifestations because I would think maybe half or a third, but 90% is like most of them.
Uh huh. That's true. So, that's why we would be, the fun fact would be really be doing a careful exam.
Right, this one really struck me a lot. And I still—I keep thinking about this one. It says roughly 25% of American adults have no teeth. Now, if it said 10% have half their teeth, I would still think that's shocking. The fact that it says 25% of adults, not including babies, have no teeth.
Can I tell one on you? I'm gonna tell one on you publicly, right? It's okay?
Yeah, go ahead.
I've gotten phone calls, text messages, and emails from her in the last 48 hours. She stunned about 25% of all Americans have no teeth.
Especially when you came in this morning and you told me that each person uses 25 gallons of toothpaste. I'm like, how is it that they have no teeth then?
I know. Well, we have a dilemma.
Anything else that you just want to point out before we get going on the show?
I guess, there’s--I wrote down five of them and some of them are kind of redundant. I guess, avulsed teeth, dentists know what to do about it, but I would think what I learned is fun facts is you could have a literature talk to your patients, assistants could talk to the patients that are sitting there, the hygienist why she's cleaning teeth could talk to patients about the avulsed tooth and the avulsed tooth, you know, we would just say pick it up off the ground by the crown, rinse it under water. Not a high spray, no scraping. Just rinse it off. And if you can, replant it.
I thought it was very interesting that it said if you can't do it right away, put it in milk.
Yeah, it's a good medium to keep the periodontal ligament alive. So, yeah, that's not a fun fact for dentists, but it's a fun fact that I think because all these moms that come in for treatment, they have kids and soccer and all these sports and it's invariable you're going to see a tooth laying around. So, if you know what to do, and extra RO time is huge, you know, like less than five minutes, not so bad. Ten minutes we’re starting to worry. There are some rare cases where people replant teeth in over an hour and they have still gone on to be serviceable.
Well, I guess with baseball season about to start and maybe a lot of parents might have their kids going into Little League, maybe you might want to know that in case they get hit by a pitch like [crosstalk]
That's right. So, the coach should know that fun fact.
Okay. Well, we have a really fun show for you today. Let's get going on it.
SEGMENT 1: Knowing the Difference – AI Diagnostic Software Packages
So, okay. So, it's time for another segment of Knowing the Difference. And this segment is inspired by a quote by the 18th century French author Madame de Stael, who said, “Wit consists of knowing the resemblance of things that differ and the difference of things that are alike.” So with this concept in mind, we're going to approach this segment to try to understand the distinctions between the various AI software systems that have been recently released in the dental world.
Now, I've seen for the past year many headlines and press releases and probably some of you have too, that says this large practice is going with Overjet or this other one is going to go with VideaHealth, this one's going with Pearl. And I know these are AI software packages, but I started thinking, how does a dentist choose what to go with and what's the difference and what exactly do they do?
So, I Googled this information and I wasn't finding anything and I kept altering my Google searches and I was not finding anything. Except finally, I found one thing by Gordon Christensen's Clinicians Report and that's a foundation that tests new dental products and reports the results to the profession so that clinicians can make educated choices about what to purchase.
So, I immediately got my hands on a copy of one of these. It was around $20 from his website. And that's gonna kind of serve as our guide for this segment today.
Yes, it's pretty exciting. You know, what's just looming and what's already started, but you can kind of see the ramp up. So, yeah. Well, okay, so.
Well, first of all, tell us the title of the report. It was called Dental AI is Here, Is it Hype or Will it Help?
Is it Hype or Will it Help? Always the choices. I guess, what I would say, I just want to play off of you, but the Foundation does a great job because no money's come in from corporations, all the funding comes from dentists, probably buying the clinician's report, things like that, and other services and courses. But it's a company that tests products. I don't know if you know this, but the Endo Activator was tested by the Foundation. And it goes out to like, you know, I'm making this up, 25, 30, 40 people, and then they use it for a few months and they all write down reports and send it in and Gordon gives you the summation.
So, we got excellent results on that. So, it's independent, there's no conflict of interest. And then, of course, he's playing off of like, well what's going on the marketplace? Well, you got Google, you know they have their, what is it called? They have their AlphaFold for proteins, you know, and we have Autopilot for Tesla and we have ChatGPT and we have OpenAI.
So, this is really started a massive conversation that has trickled right down into dentistry. As we've talked about on previous shows, we've looked at AI-defined carries and some fractures are noticeable. We've also seen some of the software that can prognosticate orthodontic outcomes. You know, even prognosticating not only who's a good candidate for an implant, but who might get Implantitis. I thought that was a fabulous thing we did. Pat on the back for us, right?
Anyway, the thing that I'm seeing now is we have to learn how to integrate this into our already existing practices and in the workflow.
Yeah. So, if you're a dentist right now, you probably have some opinion about AI. Maybe you don't doubt its ability to optimize practice management, but you're a little suspicious about how it actually can make you more productive clinically. And just in the last year, there are now several FDA-approved standalone AI software packages available to purchase, and they're for carries detection. But they're by companies like DEXIS, Henry Schein One, Overjet, Pearl, and VideaHealth are the big ones. There's some others.
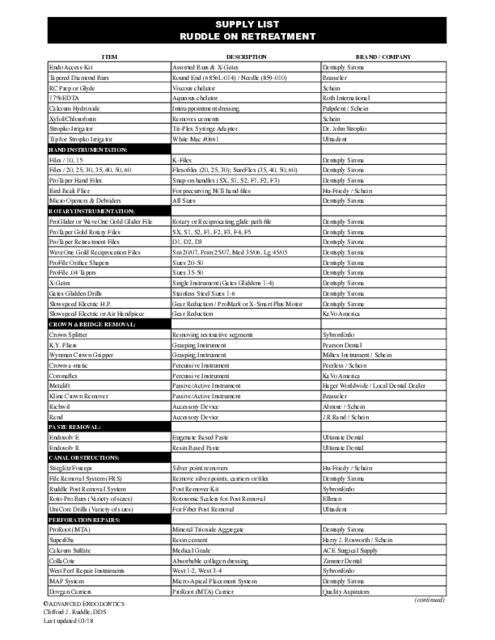
So, why don't you tell us—well, we have a graphic let's bring it up, it's kind of our—yes, okay, thank you. And so, why don't you tell us first like, about these companies’ software packages but focusing more on the commonalities.
Well, what have I noticed? Boom. I think dentists are going to probably say, I noticed the cost. [laughs]
Right.
And you can see that they're somewhere in the range of $200 to $600. And so, the expense is always going to get the attention of a dentist.
So, it's a monthly subscription.
It's a monthly subscription to get the software. And so, as you already mentioned, the carries can be looked at. But some of these things are getting, the software is getting more sophisticated. They're looking at shapes of teeth and pulp and roots. Others are looking more like, I call it lesions of endodontic origin. I'm not real familiar with all these codes because they're not codes we used in our office. We had a rule in our office, if we use codes and we use lots of codes, everybody has to understand the language of the codes. So, I'm not real familiar with the codes but I think you can just put this on pause and if you can look into this you can see some of the more critical distinctions.
But the idea is basically most offices have a computer that holds all their radiographs. And then, you buy the AI software, whichever one you decide, I have an opinion, you do too. And it runs AI on your radiographs while you're doing something else. And what’s really good about this is, you’re working over here, but behind the scenes, this thing is going on to identify things that maybe were overlooked, maybe things that aren't visible and you didn't see, but the computer calls out areas of interest.
And there's even color boxes, there's different colors that call out either carries or maybe a poor marginal adaptation under a restoration. Lesions, I already mentioned, but lesions could be periodontal lesions, calculus like that. It could be lesions of endodontic origin or maybe pick up a lesion like David Landwehr talked about that is non-odontogenic.
Okay. So, looking at this table, the first three are a little different because they're a little more limiting, because they require you to have a specific imaging system already in place. And so, that would be important to know before you purchase it. And then, you can see that there's two by DEXIS. And Clinicians Report notes that the DTX Studio Clinic might be the one to go with, because it can integrate—or what does it say? It can integrate the 2D radiographs with 3D cone beam and 3D data scans, whereas the other one, the DEX-Assist, can only analyze 2D radiographs.
Now, that's cool for an endodontist out there because if you're endo, you probably have a CBCT, you probably might--even if you're doing implants, you probably have an oral scanner and they have 2D. And so, I like it when you say you can look at all those, put them together and see things that maybe any one of them doesn't disclose.
But you would have to have the imaging systems already by those companies in place.
That’s right.
So, the other—the bottom three on the list are a little different because they can integrate with a lot of different imaging systems. So, why don't you tell us more about the Overjet, Pearl One and the VideaHealth.
Okay.
Because these are a little different.
Yeah, they--well, they all look at radiographs and they're probably, their hero application initially out of the box is my impression--now, this is all new, was carries. So, they could all find carries. And they could even, some of them can even like, well, Pearl and Overjet--well, I think all of them can even map it out and put little call outs on your x-rays.
So, while you're practicing over here, this is happening over here like I already said, but then it's not just look at Tooth 14 because there's something--no, it puts a box around and it tells you where you should go do a little more digging. And one of the big problems here with humans, which is going to make AI go, I'm pretty sure, is we're all human and we all can see colors. And there are 50 shades of gray on a radiograph at least. So, we don't have, as human beings, great distinctions of seeing these subtleties. AI can be trained to look at each and every pixel.
And I liked how some of them could--well, I think Overjet and Pearl both have segmentation, few words about segmentation. Segmentation is there's a box that calls it out, you're over here working, you go and you say there's a box there, why should it be a box? Well, then you can use segmentation software and it will now tell you this area and it'll change the pixels, it'll change--it'll do colors to distinct between different things, anatomical structures, pathological structures. And I thought that was really cool that while I'm working somebody is giving me a second opinion because I'm human and I might have missed something.
I really liked how these bottom three can look at the last 18 months—
Oh that's cool.
--of radiographs to track the disease progression. Now—
Can we say that's a recall system?
Pearl and Overjet apparently do it automatically. VideaAI does it also, but you have to do it on command, I guess.
Yeah, there’s--I'm not calling out all the things that would have been really thorough in the script, but you know, some of them, the bottom line is be sure your radiographic package, your system that you're using in your office is compatible with whatever you're looking at. That would be Step 1. Then if it is, then explore what you actually do specifically as a dentist. You might not need some of these other features, but if you're an endodontist, you're gonna want to look at your CBCTs, your 2D radiographs, right, and your oral scans.
And now, I just want to point out that we were talking about how it can track the last 18 months. Well, for Pearl, though, that is an added cost, like it's an added feature. So, you might want to also inquire what is included with your cost and are there added features you can add, that might be a question you want to ask.
Yeah, because you can take one that looks cheaper and you go, well, I'm gonna go with that because it can do quite a bit for me, but not everything. But then you find out after you got it that like, maybe I have to--I really am using my 3Ds. I really do want those scans and now there's a bump for another price. So, maybe if you compare feature for feature back here, maybe the price distinctions are not as much as we think.
Okay. Well, I think this helps a little bit as far as accuracy comparisons across the different products, now that--that research is not really available yet because the products are still really new. But in a year or two or whenever more research comes out about how accurate these AI software packages are, one thing that I think that you can pretty much count on is that they are probably going to conclude that AI assisted and a human assisted by AI does a little bit better than just a human alone. That's probably a given.
I would disagree with you, favorably in that it's probably going to make a lot of difference.
Okay.
Because I made a living--I made a living in Santa Barbara doing a retreatment and I don't know how many times the note came over with a periapical film. I don't see anything here, would you please evaluate the upper left quadrant. My assistants took pictures and before Ruddle ever saw them, they often saw frank pathology that the referring office didn't see. So, when I hear we might find more things, I am really sure you're gonna find a lot more things and just for you that are worried about the cost, you know, the money--my wife yesterday had a little tiny procedure done on three teeth. I hit her in the face accidentally on purpose and there was some minor chips from that accident. There's no lawsuits and no pending divorce I think.
Anyway, she went to the dentist, he did a fabulous job and it was $600, $600 and $600, that's $1,800 for three teeth. So, when I hear about one tooth is maybe what? $600 bucks?
Yeah.
I think if you find one single thing in 18 months and review on one single patient, you paid for it.
Yeah, that might be true. Okay. So, some of the questions that Clinicians Report ask themselves when they're evaluating products is, is it better, is it easier, is it faster, that kind of thing. So, let's go through these really quickly.
Okay.
So, AI carries detection. Is it faster?
It's way faster because, I don't want to get off on a big deal, but anyway, it's as fast as the speed of light, so it's way faster.
But you're obviously going to have to learn how to use the system so it might be a little slower.
That's gonna always be the thing is you're gonna have to learn how to use the software. You're gonna learn how to just casually like you'd look at a regular old film, look at your AI and become comfortable but yes it has to get into the workflow.
Is it easier?
Well, you were telling me that one of the FDA requirements on all AI people was to generate software that is abundantly easy for the end users to use. So, I would have to say it is easy, since that was such a big emphasis. Again, you're going to have to learn how to integrate in the workflow. So, you've got to have people savvy. So, don't try to take the person that sweeps the floors and tell them this is their new job, you take people that already are interested and they have proclivities for digital stuff and they'll probably just fly.
Okay, is it better?
Well, right now, Gordon and I would probably say it's better. From what I can see, I think it's definitely better right now, even if it's considered a little bit crude.
Okay. I think it would probably be better definitely if you're trying to follow watched lesions, like over, because of the 18 month ability to—
The progression.
Yeah, so that might be—
I want to come back, it shows--when she mentioned 18 months, it'll show you something 18 months ago and you can see if it's, you know, changing and any change off that baseline is diagnostic.
Okay. And then, ultimately will it be more or less costly?
You know, of course it's more costly and that's what dentists look at, but you always have to look at what do I get in exchange for the cost? What's the value? The value is, first of all, you might be helping people. That's kind of a noble idea. The second thing is you might keep people from having flare-ups because you're a better diagnostician. I don't think it replaces you, I think it helps you and it's like a second opinion that I've said about three times today. So, I think if you think of all those things, it's just working and laying in the background and I think as you learn to get more comfortable, it's going to be a big value.
Okay. I think that--see this is just for carries detection. I start wondering like do you have to then get another subscription for if you want fracture detection, another subscription if you want to optimize your practice management, another subscription if you, you know, want to be able to predict.
Oh, you mean like I want to watch the Raiders, that's over here, the Dodgers, they're over here, the Lakers are over here. Yeah, and I have everyone's a different package for a different monthly fee.
Yeah, if you think of just your streaming services, because I'm thinking if I could see all of the little costs that I pay for every streaming service all together in one bunch, I'm wondering actually, am I going to be surprised at how much I'm paying a month for TV?
So, maybe developers should be thinking about the end users.
Okay. Well, yeah. So, bottom line is, do you have any closing remarks about where we're at now? And should you be just hurrying up as fast as you can to try to get one of these software packages in your office? Like, what is your word for clinicians out there?
I think as you begin to think about how it can help you, we'll look at those early adopters and out of the pool of early adopters in any technology, there'll be the really early, early adopters. Well, that's who's using it right now. I didn't realize it was MIT and Harvard that did Overjet. Should I write a big check? They're taking monies; they've raised $590 million.
Lisette:; Wow.
So, anyway, as the second wave of early adopters comes in, I think we'll begin to see the edges of the truth and then I think the research will be done and when she does a Google search, they'll be head-to-head comparisons. And I think when we get there, a lot of dentists are going to have this in the future, just like all endodontists now use a microscope, but they didn't in the 70s they didn't in the 80s.
Right, I mean, I was just talking to you that there's probably a very small percentage that just can't wait to get this in their office and try it they're so tech savvy that would be like my son Isaac.
Isaac would have had it up three years ago.
Yeah. And then, there's probably some that say I will never use AI ever. There's that group, but probably most of the dental profession is like thinking well should I be buying this? What's going on? Like, what's the research showing? Like, they're just a little unsure and how do you know the difference? Well, I think that as the research comes out, like you said, there will be more side-to-side comparisons and you'll be able to, you know, maybe choose easier.
One thing to come back to something you kind of said earlier, acceptance. A lot of times--I was reading when I was getting ready for this assignment, because I'm learning just like all of you out there, patients really like this. When you show them the little blue boxes and the gold color for the carries and you show them another color for, they really think that's cool. I mean, they can relate to like, wow, this is really helping the doctor. So, I think your patients are gonna go for it.
Okay. So, maybe share that with your patients if you do have it. Show them.
Absolutely, you have a microscope, it's not a secret, is it?
Okay. Well, thank you for the information and hopefully all of you maybe are a little more clear about what the differences are, what is even available. So, thank you.
SEGMENT 2: Removal of Traditional Paste Fillers
With Ruddle, it’s Ruddle at the Board. But first, I hope you're all doing good. I hope you're off to a really good start in Q1. And I'm here to talk about something that is probably declining in popularity, but still you see it and that is called paste removal.
When I first started practicing for context in the mid-70s, I would see a case paste a week, at least one a week, okay? Within a few years I was seeing one or two a month. And then finally, I would see one occasionally. That probably reflects that there's a lower incident of colleagues using paste filler as their obturation method. So, what I want to say is a little opening remark about this. A lot of it came when endodontics knew less. We were thrilled when we got results, but there was still a lot of mysterious things that were advocated to help us maybe do what I would call today as deficiencies in primary treatment.
In other words, when I was in France, I used to watch a dentist do a crown prep. There might be a pulpal horn exposure. They would then maybe squirt paste into the pulp chamber only and what came back out after squirting in, what came back out when it was clear paste color, they went right on with the restorative. There was that kind of endodontics. Then there were people that did pulpotomies. They did a little more thorough job and they would put paste in the chamber.
Then we noticed that paste started getting down into the middle one-third and when I was in Boston in ’76, Sargenti, Angelo Sargenti, one of the main guys that introduced paste worldwide, he was talking about you know if you can get past the middle one-third and even deeper into the apical one third, that'd be a little bit better. The last time I saw him, he said, it'd be good if you did instrument to length and then the paste would be more effective. But the idea was the paste could overcome leaving vital tissue and it would react with that vital tissue. Some people thought it would nullify the tissue. Some people thought that it would help the tissue all calm down. Nobody really knew if the tissue was necrotic, if it was becoming necrotic, or in fact, if it was causing resorptions.
So, we saw these cases come out of the former Soviet Union and some of them when it broke up were called Russian Red. So, we saw paste coming from that region of the world. The former Eastern Block countries were paste users. And then of course, Ruddle in Santa Barbara, I'm on the west coast of the United States, we saw--I saw a lot of referrals that got sent in to me from people that were traveling and mobile and we saw from Asia and the Pacific Rim countries. So, those are the countries that pretty much did it.
Pastes are different everywhere. Different people have different concepts of when they would use paste, how they use paste, but primarily paste cases are declining because as I've traveled the world, I've noticed that virtually every dental school is teaching gutta percha as a primary core. So that's a little background.
Now, if we look a little bit more carefully, I'd like you to look at the asterisk that just popped up here. And that asterisk goes right to this footnote. Some of you, all of you, basically in the retreatment situation, you're not excited about retreating paste fillers, why? Because the paste oftentimes was brick hard. It was impenetrable. And there were in the day, back in the 70s and 80s, there were no chemicals that were in our armamentarium that could be used like chloroform is to soften gutta percha. Like xylol is to soften, chemically soften gutta percha. We didn't really have that at that time.
So, essentially I'm using the asterisk to point to what a lot of dentists, there's a rage -- single cone. Why was it all spawned? Minimally invasive preps pretty much negated our ability to get a lot of the armamentarium in there that we used to for obturation. So, now dentists just do skinnier shapes, single cone, and they lubricate that cone and they use a tricalcium silicate type cement to fill the root canal system.
I want to point out, it is obvious if you're alive these two are immiscible in solvents. In fact, if solvents came in for paste, we still don't have the solvent for tricalcium silicate. So, everybody that's using that is assuming I have 100% success. I will never have to go back and revise at least my work. If you're an endodontist, it's not you revising your work, you're gonna be getting cases that are failing from the community and beyond.
So, I'm gonna come back at another time, I believe this season, because this is so important that the profession begins to wake up at what we're doing with the good news, bad news story on tricalcium silicates. Stay tuned. I'm sure that got you all excited didn't it, because you're probably a big tricalcium silicate user. Fine, we'll talk about it. But right now, today we're gonna live on the classic paste.
What do we know about paste? Pastes were used pretty much in a syringable or a lentulo method of placement. If you use the lentulo there was some shaping but we don't even want to call it that, let's call it instrumentation. There was a little bit of instrumenting to make some space for the paste, but there was really no big effort to get all the tissue out because the magic paste would overcome the deficiencies.
All right, So, if it was syringed in it's important to know if we divide our roots into the classic thirds, coronal, middle, and apical, the pace is going to be most dense. It's going to be most dense closest to the orifice. This is important because you can be working up here and trying to get through and trying to get a little bit deeper and a lot of times we have a tendency to give up. Sometimes that second visit is it's often talked about internationally, the second visit is magic, right? You can't find the canal, second visit, find the canal. Can't get out the broken instrument, second visit, get out the broken instrument. Can't get the paste out, second visit, get the paste out.
So, determination and desire is a big part of this. But if the clinician kind of looks at those radiographs carefully, they'll notice that there's probably a decreasing density as we go into the middle one-third and sometimes you'll find very little in the apical third or just a little bit spotty. All right? Obviously, some clinicians were pretty thorough. I'll show a case or two like that and they actually instrumented to length and they got their paste to length and it's pretty dense all the way through. Those are pretty formidable. So, that's a little bit about how you should be looking at a paste case. If I can just get another millimeter, that's the conversation that's playing between the ears, I bet I can get to length. If you think you can, you can, and if you think you can't, you're right.
All right. So, I'm going to go through these. I'm not going to read this list back to you because we're going to look at every single one of these individually, but these are the tools that Ruddle has used and incorporated for paste removal. I would like to invite everybody to go to my continuum on non-surgical retreatment and we talk about the removal of fillers and that would be gutta percha, silver points, carrier based obturators and paste removal. So, this will be a little, you know, glimpse at the much bigger picture that we get to in a whole continuum.
All right. So, if you know about the density thing and the decreasing density thing, then you might realize in the straightaway portions, you can use NiTi files. So, we can use NiTi files where it's appropriate. As an example, we used to use rotary instruments before the Pro Taper Universal dedicated instruments for retreatment were out. That--they came out I think in 2005, 2006, it doesn't matter, just about right in there. And so, before that, we had rotary files. And if we had a rotary file, we might actually take a trans metal burr on like a profile, that's one of the popular ones back in the 90s, we had profile 04s, profile 06, GTs. You could take a trans metal burr and literally just spinning, just hit the end of the file and you'll boomer it, okay? You'll put a little asymmetry in it. It's a non-cutting tip, but we want to make it active so to get an active tip, we could just hit it a little bit and that would now make it irregular and it would start to bite and grind into these tough paste.
But we intentionally made the one that works dominantly in the coronal one-third. This would be basically middle one-third. And then, we had one that could go deeper and it was basically apical one-third. It's not always that neat, but basically crown down, get the paste out of the coronal one-third before you try to get paste out of the middle one-third.
I want to mention about paste. I didn't mention it, so I should stop. When you're talking to your patients about paste removal on a failing endodontic case, especially if they've had a flare-up that brought them into you, it might be calmed down now, but if there's been a history of a flare-up, recognize there's more post-operative problems in paste removal. Recognize that a lot of that paste that was put against vital inflamed tissue caused internal resorbed defects that can be noted years later. Get in there and get some blood coming, okay?
So, flare-ups should be communicated, they can be managed, but if people don't like to know, they like the treatment plan for no surprises. And so be aware of resorptions. So, if you can get it out of the coronal one third, there's less likely that you'll be pushing paste through the foramen and then now tend to reduce the incident of post-operative problems.
All right. So, we have a, you know, a 30/09 big instrument active tip. It'll work in the stray away portions of the canal. If you look at your radiographs and it's a really thin little prep with paste in it, you probably don't start here because we're not trying to shape the canal simultaneously as we remove paste. We're trying to remove the paste, then we'll pay attention to does the shape need to be modified a little bit to facilitate complete treatment.
So, the middle one-third, 25/08 and 20/07. These are ran at the normal speeds about 300, 400, 500 RPMs. Be sure when you're coming in with your paste, be sure you're looking at those blades to make sure the color of the paste you see with your eye in your mouth mirror is the color of the paste you see on the flutes of the file. So, in other words, make sure you're following a canal and not deviating and making a canal.
All right. So, we have files. In the straightaway portions, we have ultrasonics and we've talked about piezoelectric ultrasonics many, many times. This is a Dentsply Sirona private label from Satelec. Satelec makes the best generators in the world. Notice I'm calling attention to low power. And at the end, you choose one. These have zirconium nitride coatings, double coated, so they're sanders. And in a retreatment situation, it's nice to think that all the canals are round in their cross sections, but many of them have irregularities and fins and stuff. So, you can run the tip of an ultrasonic instrument into some of these eccentricities and blast out some posts at low power. At low power.
So, you have rotary files, we've talked about. Now you have ultrasonic instruments and then files and chemicals. And they did come along. The chemicals did finally come along. I remember in the mid 70s, I didn't have anything. And then, I started talking to guys overseas and Pierre, Professor Machtou, are you listening? One of the greatest clinicians on the planet and an academic and he could do them both.
All right. Well, he started, Cliff, Cliff we made paste over here. So when we make paste, we have to be able to remove paste. So, the first ones were desocclusal, we had Resosolv. So, we had those that I was using in the 70s and 80s and then Septodont made those too and now Septodont makes these. And this is Endosolv-E and Endosolv-R. And of course, practically speaking, the clinician chairside doesn't know if the base is a eugenol based base or a resin based base. So, you might try a chemical for 5-10 minutes and if nothing's happening and you don't see any slurry of the chemical working against that compound, putting it back up into solution, you know you got the wrong chemical. So, just simply pull it out and go with the other. So, this takes chair time, takes patience, takes determination. But remember, you will be your word and you're here to treat the patient. The patient did vote for you. So, give them the best job you can do. You could refer. If you don't like to do paste, refer it.
So, we have the small size hand files. I can even go here, but you're going to only probably be resorting to chemicals once you get to curvatures. Because again, upstairs, coronal one-third, even most middle one-third, you can get pretty nice straight line access without damaging root structure and you can have an eye towards preserving dentin, I get it, but you're probably using chemicals deeper.
All right. Files and chemicals, ultrasonics, rotary files, what else? This as an aside, the producer will probably kill me, but this is my first invention. I don't even think she knows that. So, I was introduced to Pierre-Luc Maillefer. We had dinner in Manhattan in 1989-1990 and he said, gee I understand, we had just met and he said I understand you're really one of the big advocates of microscopes. Is there anything that Maillefer could do to help you people that are scopers and you're teaching scopes. It's just starting. Is there any movement? And I thought about it. I thought well always my hands were in the way, my fingers were in the way, everything was in the way, so I thought about an offset file and 30 days later I got prototypes.
So, we invented Micro-Openers to find stuff and Micro-Debriders to clean stuff. The stuff was remnants of gutta percha, sealers, resin paste, butanol based paste, you could just plain, and we wanted Hedstrom flutes, we wanted to shave and have a more efficient and active instrument. So, the only logic to this is you can bend that file and you could pull up on the out stroke, but there's no handle in here. There's no fingers grabbing that handle, you know, to make it work and all of a sudden you're trying to look down you can't see anything, right, anything. So, we got Micro-Debriders and you know, they come in different sizes, 02, 20, 25, 30, ISO color.
Okay. The EndoActivator, especially the SmartLight Pro, I told you about the research, it's come out of India by Bola. It's the SmartLight Pro EA EndoActivator is 12 times more effective than the prior version. So, if you think about that, once you get the paste out and you can slide instruments to length, recognize there's a lot of residual paste. And it's in the eccentricities off the rounder parts of the canals, it's in the cul-de-sacs, the fins, the anastomoses, and even the initial openings in the lateral canals.
So, if you can activate a solution and get it to bombard and get it to break the solution fractures, bubbles form and they're unstable because of heat and pressure. When they implode, they send out shock waves and the remnants of that are all these little pieces of this red paste. It's still in there. You don't want to pack it. You want to get it out so that you can now go to sodium hypochlorite and now you can have clean walls that the irrigant can theoretically exchange through.
And we can use these very solvents with a concept I introduced decades ago, wicking. Wicking, watch the paper point go in. So, you got all the paste out, you think you're about ready to fit your cone and pack, but why don't we wick? So, put the paper point down in there and watch how it wicks up, it wicks up, it pulls lateral to central, off the walls, and then up the cone to pull it out. And I'll do that, I'll keep flushing with another, dry the canal, flush again, dry the canal, until the paper points are clean, white, and dry. When they're clean, white, and dry, I'm ready to go to sodium hypochlorite and do something else.
Okay. So, we've gone through the tools, and there aren't very many tools, are there and you might have discovered a couple other things, but basically, that's the main things that would be coming to mind in today's world currently 2024, if you're going to remove paste. And fortunately, paste cases are declining.
Let's look at a clinical op real quick. You know we got the access, doesn't matter what the radiograph was, I'm just showing you a tooth that has brick hard resin paste in it. We did not have these instruments. Today you would have an Acme file. So, back then, I didn't know this trick. I discovered this later. Teaching. When you teach, you learn a lot. So, anyway, notice this Profile 04. It could be an 06. Notice it's not just drifting through easily, like a hot knife through butter. It's not really doing much. There's a little bit of debris on my flutes. This is why you need an Acme tip, especially when the radiograph evidence suggests the canals are pretty straight, then you can use an Acme tip in the straightaway portions. But I said that a lot of times haven't I?
Look at the flutes. I've talked about this a lot. Look at those flutes through your microscope, objective lens, or through your mouth mirror. Look at the flutes. If the flutes are the color of the paste, you can continue. Recognize that no one file would be used to length. You'll use a bigger file generally in the bigger parts of the canal from one-third. You might drop to a smaller size file in the body. It's more appropriate for maximizing residual dentin. And then, you'll need something far more flexible and a smaller profile on its taper, a smaller D-0 that will make the curve and get the length. So, that's a little bit.
So, we are done with that. We just learned you could do this. So, you can start to irrigate with your chemicals. Be sure you have your syringes tagged and labeled so when the assistant is passing over it's not alcohol, it's not water, it's not gin and tonic, it's not sodium ethyl chloride, nor is it EDTA. Nope, it is an Endosolv-E or Endosolv-R. So, you keep wicking until the canals are dry. And then when they're dry, all emphasis, if the shape is pretty good, then the all emphasis is on disinfection three-dimensionally and then filling root canal systems.
All right, we're almost done. Just look at three cases. I told you that sometimes in other countries, I wouldn't be surprised if I would say in this country as well. People were doing restorative dentistry, they were working right along and all of a sudden they saw red or there was a pulp exposure or there was an old previous pulp cap and they chipped that out, they're in the pulp, they would just squirt paste in and go right on with treatment. And when I say go right on with treatment, I didn't say excellent treatment, this is like completely, this was dentistry done for laughs. It's dentistry that's bound to be repeated.
If you look, I mentioned the flare-ups, didn't I? Did I not mention the flare-ups? You have more potential for flare-ups. I said you have more potential for resorptions. And I said—and I didn’t say, you have calcification. Calcification. When you squirt paste against vital tissue, that tissue starts to narrow. That tissue starts to pull down and you begin to see remnants of canals, wild apical third, it disappears. We expect something there. We probably see it better if I got all the writing out of there. Just the root looks like it stops about there. So, that tends to suggest that we have different curvatures.
Take different views, treatment plan for no surprises. The crown is out of there. You know, these are two hour cases. You know, I'm not embarrassed to say back in the day, sometimes they were three hour cases. I hear young kids, they'd be, gee, I had to reappoint. Yeah, because it wasn't done yet, right? So be your word and do it right. If you have to reappoint, you know, there's a wonderful log by Kami Farris on the AAE discussion forum and it's all about what we're just talking about. Going back to get an MB2, she could not get through. On a second visit, she reappointed. The staff was dejected that she didn't just go to surgery and she got through it. She said she did a dance and then she told everybody on the forum, well, it wasn't a real dance, it was a dance in my head. All right, but that's how excited you get.
So, we can isolate the tooth, we have a full chamber for our reagents. We can get nice shapes, nice smooth flowing shapes, but does it work? So, you look at these lesions pre-treatment, you look at how large these lesions can be and you watch the inevitability, the capacity of the bone to heal is terrific. Notice in this view we have two portals of exit right here you would say, oh Cliff, merging systems one apical portal of exit. Take the other view please.
All right. So, things work. I left a post space for this dentist and of course he thought placing a pin would be probably really exciting because we can all worry about a fracture now, but right now the bone is looking very, very tight. You see that? But the bone looks very, very tight in that furcal area.
Another paste case. Okay. So, I showed you what was the pulpotomy was pretty much confined to here. This guy got paste pretty much, you know, apexes down in here. This is an apex there. Geez, this is like AI. You know, we talked about AI earlier in this segment. I'm using color boxes. I'm doing segmentation on the film. Before one lab segmentation, my goodness, and I got a root over here and it goes like that. So, what is this tooth? This is a radix entomolaris. You know, you have a radix paramolaris. That's the extra root on the buccal, but the extra root on the lingual is the radix entomolaris.
So, it has an extra root and it has all the thrill of a paste. It's got big lesions and it's got proximity to the neuromuscular bundle. What will we do? We will go in there and spend two visits at about two hours each and we'll chip that stuff out. I can use some of the things I told you about because this is pretty much a straight shot. That's a straight shot. I'm pretty good to there, but now I have a different orientation. I have an angle in here, and that is an angle I have to think about, so I have to be careful what I'm trying to put around the curve.
Now, this extra root got filled. You can see at this recall, this is about six months, maybe it was a year, but if you notice the size, you can see now we're really getting small, maybe a little bit, we can do a little bit right in here, but nice PDL in there, everything's working fine. Remember, endodontics is a regenerative procedure. If you extract the tooth, bone works, extract the root canal system, leave the tooth behind, bone works.
And we'll look at the last case. Well, I got to use red on this one. This is really going to be fun. I don't see red, but I really wanted to point out the power of leaving a root behind. Oh yeah. There is the root. Let's take it away. See it? That's AI segmentation. It's starting to show you little boxes and arrows and call outs where you should be looking a little bit deeper.
All right. So, we got a silver point in one of the mesials. There should be two, right? Don't we normally think there's an MB? And don't we normally think there's an ML? Okay. So, we got probably a missed canal, got a silver point, but this was once we had one basically, a what? In the pulpotomy, first case, then we went down to about the junction in the middle, the one third, second case, third case, you can see paste almost--I think the paste is right there. So, that means it's pretty dense and it could be easier to get through.
Like a lot of the paste cases in North America had Cut-trol. So, they had that anti-inflammatory and it kept the whole material, it kept it kind of soft. So yeah, we had the same resorptions, potential for mineralizations, calcifications, and we said post-op flare-ups, but we could get it out, unlike the ones we saw that were typically offshore. So, that's the case. The dentistry isn't good either. So, a lot of these retreatment cases, it's just a whole mindset of the person who refers the case, assuming they did the work.
So, you can see this lesion. I think you can see it quite well. It's very big. I think you saw this lesion. So, post-treatment, you wouldn't think it would get any better, but I mentioned resorptions. I've never seen a lateral canal that big. That was probably a lateral canal that had tissue in it that wasn't removed and that inflamed tissue began to eat away at the canal. The tissue might have even gotten more inflamed when the paste touched it because it was like caustic, it was cytotoxic.
All right. So, I see that. You see that rope. We're using a really good sealer. Watch that sealer hold up. Watch that new bridge. It’s got a new bridge on there. And essentially again, the thing that always made it exciting for me the ability, the inevitability of the bone to come in and grow after eliminating the root canal space as a source of contamination to the peri radicular tissue.
So, that's my little job on paste. That doesn't tell you everything, but we've talked about all the other filling materials. So, the producer said, Ruddle, you need to get in there and talk about paste. It might not be as popular as it used to be, but there's still cases out there and they need conservative non-surgical retreatment.
So, what's my last call? My last call to action is, look at the graph. This isn't gutta percha, these are sealers. So, we've always used pretty much Grossman type sealers and you can see they've been, okay, I don't know what the numbers are. Nobody knows what the numbers are. The literature doesn't know what the numbers are. The numbers could be how many paste cases were treated worldwide last year? Okay, we don't know.
So, this just means increasing number of cases. You can make it, it's a concept graph. It could be in your community, it could be in another country. It might look like a little different. But anyway, we had the Grossman type sealers and they were very popular and they've been used. You taught them in dental school, okay? They started to fall off. They started to fall off a little bit along the journey because we started to see things other than zinc oxide eugenol. We started to see resin, methacrylate, we started to see tricalcium silicate sealers, so we started to see a different family.
Then there was minimally invasive endodontics. The skinny shapes led to single cone and of course everybody got really excited about the tricalcium silicas because they were regenerating materials. We're going to explore that at another time but it's taking off. So, whatever this slope is losing it seems to be replaced by that and then of course your paste cases have just been getting lower and lower.
So, I'll leave you with this. What is the burning question? What about the tricalcium calcium silicate sealers? We'll be dealing with that. Stay tuned.
CLOSE: Vintage Dental Ads
Okay. So, dentistry has come a long way in the last hundred years and you know what else has come a long way? Dental advertising. We recently came across some vintage dental ads and we thought we would share a couple with you. So, let's bring up the first one. This is for Dent’s Toothache Gum and it says stop toothache instantly. It says how to use it. Clean the cavity of the tooth and press firmly into it a piece of gum. If no cavity, apply to the gum as a plaster. So, is this kind of like what your open tooth instructions used to be back in the day?
Yeah, they've come a long ways, haven't they? Well, I saw London in this ad, and I was thinking of my London friends, like Shannon Patel and Julian Weber, guys like that, and there's many others, and I was wondering if this is one of their early patients.
This ad is, by the way, from 1902, so it's very early. It's over 100 years old.
Oh, wow. Maybe it's Julian and Shannon's parents, grand grandparents, great grandparents.
Okay. It's interesting that they also offer Dent’s corn gum, which cures corns, I assume, on your feet or something.
I'm using it regularly, not for my teeth, but for the—so I can keep walking.
I think it's funny when you see the old ads of people that have a toothache or something or on TV and they tie that thing around their head. Like I'm not sure why they would do that.
You know I—
Hold everything together.
Well, I was wondering if maybe once you have the knot tied and you have a sling maybe you can slide an ice pack or I don't know what they had in that day, maybe a little heating something in there might be soothing, who knows?
Okay. I don't know if you can still buy toothache gum. So, I don't know. Let’s look at the second.
No modern days you got to the dentist.
Okay. The second one we have is for Listerine toothpaste and this one is from 1927 and it's kind of funny. It says good news for the man supporting a family. If you are supporting a large family, here's good news for you. Listerine Toothpaste, the finest achievement of dental science, costs but 25 cents for a large tube. So, those who have paid up to 50 cents for other dentifrices can now have whiter teeth and save $3 per year per person by using Listerine Toothpaste. Think how that mounts up in a large family with everybody using toothpaste every day. Worth considering, isn't it? So, that's just really funny, I think.
Not to make any jokes, but if you think about the era, the 20s, that was the Great Depression, so you can see a guy with a family might be in the back room you know trying to figure out how to make everything stretch and anyway, he loved it gets the teeth gleaming.
The whole family can brush their teeth and everyone can have clean teeth and you can save money.
So, little things matter.
Yeah. So, I just like the idea, like they're even in this day they're saying you can save money by--and always that seems to be a constant throughout history, right? People want to save money. So, this—
Always looking for the angle.
This is the way to do it. And now Listerine, I don't know if they still make toothpaste, but I have some Listerine mouthwash in my bathroom today. So, they're still in business. So, do you have any closing remarks?
No, it's just fun to look at the history of anything cause you can learn a lot about what you're doing now and you could measure that and have that admiration for the journey. But then you also can look at where they were and where we are and you can start to look ahead and kind of see how it might go in some places.
It's kind of funny that we're talking in one segment about ads from the early 1900s and in another segment we were talking about AI.
Future and past.
All right. Well, thank you for watching and we'll see you next time on The Ruddle Show.