There are many factors that influence the long-term retention of critically essential teeth. Certainly, endodontic procedures pose treatment considerations when performing restorative dentistry...
A Week In the Life Special Guest Presentation by Dr. Cami Ferris-Wong
By now, it is no secret that Ruddle & Lisette like sports; now you can learn which sports analysts or announcers influence their thinking and why. Then, Dr. Cami Ferris-Wong, a full-service endodontist, gives a presentation on what she encounters in the average week… from trauma to restorative issues to root fractures and more! After, Ruddle and Lisette share some insights in a post-presentation discussion. The episode concludes with a very unusual Ruddle case report … Think not from an average week.
Show Content & Timecodes
00:16 - INTRO: Influencers – Sports Analyst/Announcer 09:26 - SEGMENT 1: Guest Presentation by Dr. Cami Ferris-Wong 44:00 - SEGMENT 2: Post-Presentation Discussion 55:06 - CLOSE: Unusual Ruddle Case ReportExtra content referenced within show:
Other ‘Ruddle Show’ episodes/podcasts referenced within show:
Downloadable PDFs & Related Materials
How can the dental team distinguish between a true emergency vs a non-emergency? Much of how a dental team reacts to an emergency patient is based on...
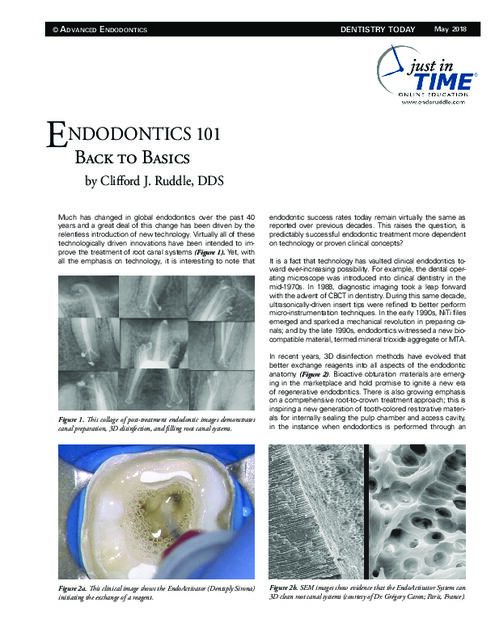
Much has changed in global endodontics over the past 40 years and a great deal of this change has been driven by the relentless introduction of new technology...
This transcript is made available by The Ruddle Show in an effort to share opinions and information, and as an added service. Since all show text has been transcribed by a third party, grammatical errors and/or misspellings may occur. As such, we encourage you to listen/watch the show whenever possible and use the transcript for your own general, personal information. Any reproduction of show content (visual, audio or written) is strictly forbidden.
INTRO: Influencers – Sports Analyst/Announcer
Welcome to The Ruddle Show. I’m Lisette and this is my dad, Cliff Ruddle.
How you doing?
Pretty good, what about you?
I’m excellent. The sun is shining in Santa Barbara, right?
Yes. It’s a nice summer day.
And of course July brings a great time for endodontic education, but also we can pause just a little bit. Tell us all the sports going on right now, just in this month.
Why don’t you tell us?
Well I know there’s Euro fútbol, there’s Copa America over here. You want to fill in a couple more?
The Tour de France is going.
Wimbledon finished. The Olympics is around the corner.
Baseball.
All Star game. I mean come on guys. It’s endodontics and we’re having a big high in endodontics in July too.
Okay, well you did mention there’s a lot of sports going on and this is kind of connected to our opening segment, which is influencers. And in this segment we talk about something that has really influenced – it could be a person too – something or someone who has really influenced us and how we think in our daily lives. In the past we talked about a childhood friend, and we talked about a favorite preferred technology, but we excluded iPhones.
So today we’re going to talk about the sports announcers who have most influenced us. So how about you go first. I think you narrowed it down to three.
I kind of went with the ones that I played growing up. I’m going to mention football, and just to be clear, I played flag football. But I loved football, baseball and basketball. So in football, it has to be John Madden. John Madden, if you don’t know overseas, was quite an athlete in high school. Then he went to where our producer Lori went, California Polytechnic Institute – Cal Poly. And then he went into coaching, and then he got hired by the Oakland Raiders and he had about a 10-year run there, tremendous record. Then he went to the booth and began to colorfully explain the game so that we could understand better. And then he even got involved in what was it? Game consulting; he made video games.
So what did I learn from John? I learned that I could – he would explain things to me that I couldn’t see. I was always following pretty much the ball and the players around the ball, and he was having me look away from the ball. And I loved that, because in endodontics, sometimes when you’re playing a movie, don’t explain the movie to what they can see; tell them something in the movie they can’t see. So I learned that little trick.
Baseball… Vin Scully was music, was a storyteller, a kid born in the Bronx, a 50 or 60-some year career as voice of the Dodgers. So nothing to say except he was just – I think households all over the nation, your household; he would fill the rooms and you didn’t even have to be watching the tele. You would be able to imagine perfectly because of his descriptions. Very colorful.
I like also how you told me that he was sometimes just quiet. He just let the game breathe and you could hear the crowd or the crack of the bat.
That’s right, and a lot of people feel they have to fill all the air up. And maybe back to the videos and the lecturing; sometimes you’re playing a really great video, or an animation I should say; maybe Ruddle just zips it.
And finally so we can get to your fun stuff; basketball, the voice of the Los Angeles Lakers. Another guy, 50-60 years, started back east and then had a long career: Chick Hearn. We showed statues, right? Recently we showed statues? He’s actually one of the statues.
Yeah. I think we missed that.
Anyway, wonderful voice and very colorful. I looked yesterday beyond what you gave me some notes to look at, and all the things he introduced that were iconic, first-time used expressions. And I just scrolled; I didn’t realize Chick did all those things. Like The Big Fella and stuff like that.
But the one we liked the most is when the game was in the bag – in other words it was over, but they were still playing because there was still time left on the clock – he would say “the game is in the refrigerator.” He would say “the door is closed, the lights are out, the butter’s getting cold, the Jello’s jiggling.”
What have you got?
Well you took Vin Scully, which he might have been one that I picked because his voice is music to me. I’ve fallen asleep many nights listening Vin Scully’s voice. But probably some of my favorite announcers of all time are Phil Liggett and Paul Sherwen. And they commentated the Tour de France, which is one of cycling’s grand tours, and they did it for 33 years together until Paul Sherwen died a few years back, and now Phil Liggett is still doing it with Bob Roll. Well those who know me know that for over 20 years now, I have watched the Tour de France.
Oh yeah, faithfully.
Yes, and I’ve listened to their voices for that many years. In our house, the kids have grown up listening to – waking up hearing Paul Sherwen and Phil Liggett’s voice, because that’s what time it’s on. It’s on in the early morning here in California. And after Paul Sherwen died, Phil Liggett still does it; he does it with Bob Roll now. So not only do we watch the stages in the morning, but we then replay them throughout the day. So it’s basically on all day long in July, because the Tour is 21 days.
So everything I’ve learned about cycling – people always ask me if I ride, and no I don’t – but everything I’ve learned, the vocabulary, the strategies, the rider assignments, I’ve learned from Phil Liggett and Paul Sherwen.
He was your John Madden.
And I also kind of have learned from them – they didn’t actually say this, but I feel that this is how it is – I think the Tour is kind of like a metaphor for life. There’s the long-term goal, but there’s also the race within the race every day. There’s the mountain stages, the time trials, the sprint stages, the cross-winds and the feed stations, the nature breaks, the crashes, and even the spectators and even cheating too. So it has everything in the Tour.
It has life!
And I’ve literally experienced every emotion watching the Tour. It’s not unusual to see me crying at the end of every stage. Even if my rider that I’m rooting for is not winning, just seeing them cross the line and how tired they are and the celebration. I know it’s just the height of cycling to win a stage in the Tour, so I’m crying pretty much every day. And then just seeing the French countryside and the storytelling; I mean I just love it. I love July every year.
Well I guess I don’t have much more to say. But she got me interested in the Tour back in I guess the Lance Armstrong era. Probably pretty easy to get excited because it was an American rider. But anyway, what I liked about it – and I don’t know half of what she knows – but I like, probably when I watch golf sometimes and you see these iconic locations by the ocean and they’re golfing. I love the little villages, the narrow streets, the majestic landscaping. And then the crowds that are so close and they come in and the rider is going through a chute; I always go geez, I think somebody should be falling by now.
But anyway it’s quite an event isn’t it?
Yeah, and even if you’re not watching, just the sound of golf, baseball or cycling, just having it on the TV; for me it’s just really calm and it just makes me feel happy.
There’s nothing like the aura of the peloton.
Okay. Well we have a great show today. We have a guest presentation so let’s get to it.
SEGMENT 1: Guest Presentation by Dr. Cami Ferris-Wong
Okay, today we have a guest presentation which you will see momentarily. It is by Dr. Cami Ferris-Wong, who is an endodontist here in Santa Barbara. And while she was getting her degree in biopsychology from UC-Santa Barbara, she worked as a part-time dental assistant and developed a passion for endodontics. I’ll tell you about the rest of her journey momentarily. The title of her presentation today is A Week in the Life of a Full-Service Endodontist. Full-service means she does everything except implants.
So why don’t you tell us first before we watch, how it is that you know Dr. Cami Ferris-Wong and how it came about that we have the opportunity to show this presentation today?
Well I have a car, so every now and then I get in my car and I drive, and every now and then I would end up at my friend Terry Pannkuk’s office. And way, way back, she was his assistant, like you said. And then later, because Terry gets people excited about endodontics and she had the passion, and so off she goes to dental school, I think University of California San Francisco. And I used to teach those graduate students every year, and then Ruddle With the Residents, so I’m not sure we ever connected in that venue. But in any event, some years later, Terry and her decided that she was endodontic – should go there, and went to BU. Followed Terry in his footsteps and she got Herb Schilder, because he retired in 2000 and she was the class of 2000. So that was really – good job, you snuck that one in there Cami.
And then finally I got to speak one time here in town. There was a very prestigious alumni study club called Boston University, and they have annual meetings. And so it was the first meeting after Covid and everybody was kind of like a little concerned, but we all came together and we had a great time. We have a nice crowd and she presided over that meeting. So I got to speak to the alumni at BU, I’ve done it several times but never in Santa Barbara. So that was another time we interfaced and there were a few discussions during that; you know, what am I going to talk about and stuff. Predictably Successful Endodontics, Her Mentors; that was the title of my lecture, Her Mentors thing.
And then finally I’ve seen her on the Forum. And I’ve really learned to like her cases on the Forum, and we’ll talk about that more.
The AAE Discussion Forum?
Thanks. Because there’s maybe 3-5 people that you might call that kind lead the conversation, and others are encouraged to pitch in and give their observations. And I’ve seen her cases that are impressive. I like the way she thinks, the critical thinking part of it, and then there’s some passion that I really admire. So I thought maybe she should be on the show. But she said Dr. Ruddle, I don’t give lectures. And I said yes you do, you’re on the Forum. And she said well. And I said that’s just a case presentation; you could just show a case, a few words, next case. So here we are.
Okay, great. Well just to tell you a little bit more about Dr. Cami Ferris-Wong. I mentioned majoring in biopsychology from UC Santa Barbara, and she actually graduated there with high honors. Then she went to UC San Francisco for dental school. And then, as you said, on to Boston University to train under Herb Schilder.
Right.
So when she graduated in 2000, she came back to Santa Barbara to enter private practice. And then in 2009 she went on to become a Diplomat of the American Board of Endodontics. Her hobbies include beach volleyball, golf, pickleball, reading, community volunteer work. She’s married to Dr. Derrick Wong, who I think you said is an endodontist.
He is too. And you know, she has a lot of – I’m interrupting, but she has a lot of fun with her staff too.
Oh? And she has three daughters. So we are very excited to show you this presentation; let’s see it.
[Ferris-Wong Presentation Begins]
Hello. Thank you so much for that introduction. As you heard from my bio, I have known Dr. Ruddle since I was about 18 years old working as a dental assistant here in Santa Barbara. And more recently, we’ve been able to interact when he came as a presenter to a conference that I put on here in Santa Barbara. So over the years we’ve been able to get to know each other a little bit better, and I’m just so honored that he chose me to be the guest speaker for this show. So let’s go ahead and get started.
So first off, I am not a paid representative of any of the companies that I might talk about throughout the presentation. And again I just want to say think you to Dr. Ruddle and his whole team for inviting me, and also for supporting my practice over the years. Every now and again a patient comes in and says that they were referred by him, and that’s always fun and exciting. There’s no greater praise than having Dr. Ruddle refer a patient to you.
And then I also just want to acknowledge my mentor from Boston University, Dr. Schilder. I feel like he’s with me every day in my practice. I’m constantly thinking about things that he said and the inspiration that he’s given me to be the best endodontist I can be and just provide excellent care each and every time.
One of the things that Dr. Schilder used to say when he would be talking about interacting with other endodontists is he would say “show me your molars.” And what he meant by that was that he kind of wanted to see how the person practiced, what kind of work they did before he would really engage with them in conversation about techniques and things like that.
So I just wanted to show kind of smattering of different cases here that I’ve done over the years that are kind of fun anatomy cases; kind of interesting curvatures and difficult access and things like that. These are all good and fine, but also there’s something to be said for just what we’re doing on a day-to-day basis.
With these kinds of tough cases, I think it’s really important to keep in mind that you need a lot of patience for these cases, for the tough ones that come your way, as well as every case. Every person and every case is difficult in some way, I find. It might be the tooth is easy, but the patient is difficult; it might be that the patient is easy, but the tooth is difficult. But having patience, giving yourself time, making sure that you’re not rushed really allows you to do your best work. Being persistent in cases that are difficult, not being afraid to close up after you’re a first visit if you weren’t able to negotiate all the way or there was something that you felt you could do a little better. Having the patient back a second time oftentimes makes things a little bit easier to get into for whatever reason. Having a little fresh energy is not a bad thing on a second visit. And going back to those pre-curved hand files. Even in the world of rotary instruments and advanced irrigation, a good pre-curved hand file comes in handy when trying to get into some tight spaces.
So when thinking about what I wanted to speak about for this presentation, I had a lot of different things I wanted to talk about. And then there was one week in May where I had a plethora of different cases all come in on the same week, so four days, and I thought this is what it’s all about in endodontics is that there’s not just root canal through root canal through root canal. It’s all these different types of cases that come in, different types of patients that come in and how we handle them. And so I thought I would just go through literally one week. And the other thing about this is that I didn’t take my best restorative case and my best retreatment case and my best surgery case to show you. I’m just showing you the ones that walked through the door during that week. So this is just not curated or anything like that; it’s just what I saw during this week. And that way we can kind of touch on a lot of these different things.
And I do call myself a full-service endodontist to my referrals, which means that I basically do anything having to do with endodontics. The only thing that I don’t do is implants. And so they know when they refer to me that I have all these tools in my tool box, and that if I can save the tooth, I will do my best to do that. But I also understand when it might not be the best thing to save the tooth. Even though I don’t do the implants, I do refer a lot of patients out for extraction and implant.
So the first thing we’ll talk about is restorative. I’m a strong believer in the fact that I believe endodontics – sorry, endodontists should restore the teeth that we treat so that we are giving the tooth the best possible chance at success. Because I feel that the tooth will never be as clean as it is that moment that we have it under rubber dam and we’ve gone through all other cleaning and shaping and advanced irrigation if that’s what you’re using. And so this is one of those cases where I did the restorative as well. What I do in my practice is if there is an old filling or a crown that has recurrent caries, I want to get everything completely cleaned out. So if there is a crown that’s leaking or has an open margin, that’s got some recurrent caries, at the consultation visit, I’m explaining to the patient that they’re going to need a new crown and showing them why, and then going through the steps of what we will do to get them prepped so that they can go straight to their restorative dentist. And by straight, I mean within a week or two is ideal on these cases to get them in and get the crown done.
So with this case in particular, we always take a pre-op quad impression so that we have a putty matrix for the restorative dentist to use if they want for a temporary. I remove the crown, remove all the caries, and then I’m able to really get into the canals easily. I feel like the cases actually go a lot smoother if you remove the crown and all the caries and all the restorations. You get to see if there’s any sign of any fractures, document all of that, find all of the canals a little easier and so forth. It’s also better when you’re working with advanced irrigation, because especially with GentleWave with the high pressure, any leakage under a crown you’re going to have issues with the irrigant solutions leaking out potentially into the patient’s mouth. So just making sure that everything is shored up with the caulking material, the sound seal. It just makes you feel very comfortable that it’s going to be predictable and that you’re not going to have any issues with the advanced irrigation.
So then you just make it easy for the general dentist. You just create this nice margin here. If it’s a really deep margin, I’ll oftentimes use a blue type material so that they can really see that margin easily. And I just let the patient know; it’s going to be like a little mini tooth for a week or two until you get the crown. Be careful with not chewing over there as best you can, keep it nice and clean, and then by the time they get into the restorative dentist, the gingiva is all healthy and happy and it makes it a real easy appointment for them there.
So again, these are just the cases that came in that week, so I’m not showing you my very best molar case. You’ll see there’s a little extrusion here. I’m not worried about that, but at the same time, this is kind of a standard kind of case that you’d see in my practice.
So I do like to treat kids, and I know a lot of endodontists don’t necessarily like that part and a lot of them don’t see kids unless they’re a certain age. I don’t have any particular age minimum. I see any patient that has a permanent tooth that needs to be looked at, and then I determine if the patient can be seen with or without an anesthesiologist coming in. And most of the time we don’t need an anesthesiologist. My staff is really good with kids. I’m adamant about seeing them for a consultation first so that I get to know them, I do the look/tell/do, show them the mirror that I’m going to use, tell them I’m going to look at their tooth then do it. I tell them I’m not going to surprise them with anything and they can always raise their hand if they need me to stop. Just developing that trust at the consultation visit I find that they come back for treatment and do really great.
And so I have a trauma case here that I’m going to show, working with a 12-year-old child who had a trauma from a snowball accident. And when you’re working with these trauma cases in particular, you’re dealing with the patient as well as the parent, of course. And one of the biggest things I find is that the parents and the patient are oftentimes really anxious and worried about what this is going to look like for the long term. So the first thing I do after I sit down with them, before I even take a look at their mouth oftentimes I’ve already taken a look at the CT scan and I know the situation. And I’ll say okay, here’s the situation. And I’ll let them know in a case like this, she may not keep the tooth forever, but that we’re going to try to keep it as long as possible. We’re hopeful that she’ll be able to have normal growth, normal development, and when she’s an adult she might need an implant – we’re not exactly sure when – but that our main goal is to keep a healthy root and healthy bone for as long as possible.
In a case where there’s not a fracture like this and it’s a trauma case where I feel very good that the tooth will be successful, the very first thing I’ll say is you’re going to be okay, the tooth is fine, we just need to do some things to treat it, make sure it’s healthy, but you’re not going to lose this tooth. And I feel that people just take a deep breath after that and they can actually listen to what you have to say. But up until you kind of tell them whether or not they’re going to keep their tooth, they’re not really listening to anything you say.
So for this case, the dentist saw the fractured tooth and splinted it and then sent her to me. So it had been a couple days since the trauma when I got to see her and do the CT scan. And I said all right; let’s see if we can just save this tooth as long as possible. My goal was to get the tooth treated and get a post in there so that there would be internal splinting, and then eventually we would most likely need to do some rapid extrusion when she’s in orthodontics, knowing that that fracture line would probably an issue.
So we went ahead and went in and did root canal treatment on the tooth. The actual isolation for the obturation wasn’t a problem, believe it or not. I was able to get it dry and get it sealed off. But when I went to put the post in, it was a problem, because I wanted to push the coronal segment back up and approximate it as best I could. It had loosened up a little bit over the course of just drilling on the tooth and working on the tooth.
So I was pressing the coronal piece up, I had the post fitted and I was getting in the cement and trying to get the post in, and meanwhile there was bleeding coming in from the gingival sulcus and it was a bit of a mess at this stage. So I did the best I could and this was our result. It didn’t have any mobility when she walked out the door. She was happy, mom was happy. I wasn’t super happy with how it looked and how it went at the end, but we said all right; let’s kind of see how this goes.
Well, a week later she comes in and says the tooth is a little bit loose again and kind of bugging her again. So I said well let’s set you up for another visit. So she came back in again and I drilled out the post. And this time, because I had already reapproximated the pieces, I didn’t have any issue with isolation that second time around.
So again, just being patient about hey, we’re going to do the best we can each step of the way, and with the understanding that we might have to do something more than we think. We may have to see you more often than we think. But they were very appreciative that I was willing to go back in and do that post again.
So then here we were; she came in during that week in May for her three-month recall. She’s asymptomatic, there’s no mobility, she’s being careful not to eat on that front tooth, which is what we told her to do. The only real issue is that she’s got this little line on her gingiva which is consistent with where the fracture line is. But it doesn’t bother her and so we said okay, let’s go ahead and give it a little bit more time. The next step will be for her to get in to the orthodontist and start looking at doing ortho. And so as a part of that, we may start to do some rapid extrusion to bring it down so that that area of the fracture is not irritating the gums anymore. So if we get it just a little bit further down to where it may be slightly subgingival, and if it’s an issue, I can even raise a flap and do a little bonded composite to seal it off if that little crevice is getting plaque or bacteria in it, that kind of thing.
So they know that there are kind of multiple things that we may do along the way. And again, just the main thing of keeping this root as long as possible.
So the next thing I want to talk about is the resorption that we see, which is a lot. But of course there is internal and external resorption, but I find that true internal resorption is actually pretty rare. Most of the cases that we see are external resorption, and whether or not we treat them has a lot to do with whether they’re symptomatic or not. But also the location of the resorption and then also the tooth location. So the strategic value of the tooth; how hard is this tooth going to be to replace with an implant.
And then the other question in my mind is always well what if we do nothing? So a patient like this, 68-year-old female. She doesn’t have any symptoms, she has a new dentist in the practice that she’s going to and so the older dentist retired. So the new dentist saw something on the radiograph and said let’s get this checked out. She came into my office saying I don’t know why I’m here. I don’t have any symptoms, nothing has changed in the last few decades or what have you.
So we did a little detective work as far as asking historical questions. She said that she does remember the retired dentist watching this area for as long as she can remember, so it wasn’t the first time she’d heard about this. And then when we did the pulp testing, she did say she felt some cold which was surprising given the amount of calcification she had there. But I double checked with the electric pulp test, and sure enough there was some vitality there. So without a necrotic pulp I didn’t see any reason to do root canal treatment on this tooth. I said it may be changing over time, it may be the same as it’s been. We requested some old radiographs to see. And so this happens quite a bit where we do a little homework and ask for some old radiographs; and sure enough, they looked pretty similar. So I did tell her if she wanted to recheck it after a year we could do that, or in five years. She declined and said she’ll just have her new dentist keep an eye on it.
But there a lot of cases like this where really just watching and waiting is the best option. Or a case where doing the implant is not an issue, then just watching and waiting until it becomes a problem, and then having the tooth out and doing an implant. But it depends a lot on where the resorption is, how accessible it is, and how motivated we are to keep that tooth.
So here’s an external resorption where we did decide to treat it, because it’s a front tooth and it’s already starting to get pretty close to the pulp here. This is what I’d consider a Class III-ish resorption defect. And so this gentleman is 75 years old and they are starting to get into that defect when the hygienist is cleaning. So she felt that hole under the gum and they sent him over. So he doesn’t remember any history of trauma, but there’s something going on here and we decided we did want to address it before it got any worse.
So on these cases, if it’s a Class 1, if it’s small enough, I’ll just do the resorption repair without doing endodontics. If it’s Class II possibly as well, and especially now that we have vital pulp therapy in our back pocket, I will think about maybe even just doing a resorption repair and a bioceramic pulp cap if we do end up exposing the pulp. But areas like this I find to be a pretty big defect once you’ve cleaned it all out, and I worry a little bit about the structural integrity of the tooth as well. So not only am I worried about exposing the pulp, but also the long-term success of the root.
And so I’ll do a three-part approach on these cases, where I first go in, I access, I place a gutta-percha cone passively in there and a little temporary filling. And then I lay the flap. And this is what the defect looks like before I’ve prepared it. So it’s already pretty large, right down to the osseous crest there. And so when go in and clean out the resorptive defect, we’ve gotten pretty deep in here. I did do just a little bit of crown lengthening there. And interestingly enough this one did not end up in an exposure, but I felt that it was good to have that cone in there just in case so that I have something to put the restorative filling on and I don’t block myself out from the internal aspect of the root canal process.
So once I place my restore composite and then I flap the tissue back and suture it up, then I just go back and do a regular old root canal treatment. So get the obturation done and then bond in a carbon fiber post, and this is the restorative that I placed surgically.
So that all went really well. This is just to show you a similar case that I did three years prior. This is the recall showing how nice the bone looks and the filling, and this is how nice the gingiva looks and this patient is asymptomatic as well.
So I also had an interesting retreatment patient come in that week. He came in with just a referral slip that said eval 8-10 for retreatment. So I didn’t really know what the plan was in this area. It’s obviously heavily restored with fixed posts and these lesions here. His general dentist had done the root canals and the restorative over 20 years previous, and #10 here had been retreated by me 10 years ago. And so when they said eval 8-10, he had seen the CT scan and was a little concerned about all three of the teeth. So here’s the CT of #8; you can see the small lesion there. Larger lesion on #9, as well as some resorption, root end resorption. And here is the CT of #10, but what he didn’t know was the history of #10.
So I first saw him back in 2014 for this large lesion, and we at that time had decided to go through the existing crown, remove the post, and do the retreat. So here’s the one-year recall, and you can see how much better this looks. And at the time in 2014 I hadn’t been doing CT scans routinely. So I don’t have any scans of this lesion, but I suspect given how large it is, it’s quite possible that it could have been a through-and-through lesion.
And so when I see this scan, when I see this result at 10 years from here to here, and I see this scan looking like this, I don’t worry about how it’s a little bit darker in here; for a couple of reasons. One is if it was a through-and-through lesion, this may be a little bit of a scar. And we do have the cortical plate here looking intact. And as I went through the scan, this looked like it could be a little bit of just a normal trabecular pattern as well. So without any symptoms and with this kind of healing, I told him I wouldn’t worry about tooth #10. But we did need to worry about #8 and 9.
And so I called the dentist and said what’s the restorative plan here? Because I would like to retreat these, but I’m a little concerned that going back in and removing the posts, the crown and/or bridge abutment might loosen them or come off. And he said that’s fine; we’re thinking about doing all new restorations in the near future as well. So I said that would be my preferred way to go about it, so he told me to go on and do that. But definitely this case was one where I wanted to communicate with the general dentist, because what I didn’t want to do was just blast in and start doing retreatments non-surgically and upset this whole restorative apple cart if the dentist and the patient weren’t on board with the possible whole reconstruction that would have to go on here restoratively.
So we do plan to see him back for a recall exam before he does any restorative work, and he does know that there’s a possible need for apicoectomy in the future, particularly on #9 with all of that root end resorption that was a real irregular shaped portal of exit. That’s a little difficult for me to maintain the filling material there, but we’re going to keep our eye on these and he understands that there’s a possible need for surgery in the future.
And speaking of surgery, so we’ll go through. This patient came in on recall, but I’ll go through the sequence of events leading up to that. He was 35 years old, he was a special needs patient, so he kind of was flinching when I would go to touch him. He didn’t communicate really, he doesn’t talk much. He came in with some palpation soreness and a draining sinus tract. The tooth was discolored and his mom was with him as well. And though he couldn’t communicate well, she said that she really wanted to lighten the tooth up. So I said well, we could go ahead and do a retreatment and internal bleach, but most likely we’re going to end up needing surgery on this tooth. But they were fine with that and so we went ahead and did the retreatment. Really large apical foramen here, so knowing that I was going to go back and do the surgery I went ahead and packed bioceramic putty in the apical area here, and then bonded in a post.
So when he came back at three months, he was asymptomatic and had no mobility. He was being careful not to eat on the front tooth as much as he could. And then we saw him at six month and there was a sinus tract back. So it had returned about a month prior to us seeing him at the six-month recall; otherwise he was asymptomatic. So I said let’s go ahead and go in and do the surgery.
So when I went in, I went ahead and resected. I didn’t have to do a retro prep or fill because I already had the bioceramic in there, which any retreatment case where I suspect I’m going to need to do apical surgery, I’ll always try to do that where I go ahead and place the bioceramic cement at the time of non-surgical retreatment.
So I went ahead and resected this back to the level; I kind of went on an angle to just mirror what the lesion looked like. And then we did what I call kind of a sandwich technique. You can see here where it’s through-and-through, so I placed a little bit of membrane there, and then the graph, and then the membrane on top. So it’s membrane, graph, membrane from the palatal through to the facial aspect. And here it is right after treatment.
So when he came in that week in May, it was our one-year recall, so this made me very happy. So side-by-side CBCT, so this is pre-op and this is one year after surgery. Here it is with the radiograph and then a couple of side-by-sides. I do find that on the 3-D rendering a lot of times it will look a little bit dark there still. But you can see here on the actual slices, it looks great. And this is how it looked in the mouth. It was really grey pre-operatively before the bleaching, so they were very pleased with the cosmetic result as well as the papilla and the gumline all looked great.
So we see a lot of patients come in of course with cracked teeth. Wondering whether these teeth can be saved is a big part of endodontic discussion, especially in our endodontic forum about cracked teeth. I have to say the CBCT is the very best thing diagnostically in my practice in the last 10 years, because of being able to have a better idea of prognoses on teeth that have fractures. So I do a CT scan basically every tooth. There’s the rare ones that I don’t, but pretty much everyone that comes through my door gets a scan. And I can’t tell you how many times I’ve been so thankful. At least every week I see one where I go I would never have seen that or never suspected that. It makes cases go a lot smoother. And also using advanced irrigation; just knowing the anatomy, knowing where the inferior alveolar nerve is, on maxillaries knowing where the maxillary sinus is is just absolutely critical.
So in this case the CBCT saved us from a bunch of extra treatment on this patient. He’s a 49-year-old, came in with constant throbbing, it was an emergency visit. And he had just had the zirconium crown placed two weeks prior, but again a little dental detective work. We know what’s going on with the crown, what happened before. He basically told us that he had a crown on before and that crown had fractured. Asked about any history of fracture before that and he said oh yes. The crown was put on because the tooth had fractured, and so the red flag immediately goes up. And so on the CT scan we’re looking very closely, and of course we see this little isolated defect right here. It has a perio probing of about 7mm that was consistent in that area.
And so these cases I feel like are so helpful for us as a profession to be able to diagnose before we do the endo and end up having them come back with pain and swelling and problems later, and then they think the root canal failed. So I’m very thankful for the CT for this, but also that I don’t have to go in and do an access explore for fracture, one hour or one and a half hour visit to find this out. Because on the regular radiograph and just with a regular probing, I probably wouldn’t have found this isolated defect.
So I’m just really thankful for the CT scan, and I tell patients that. I say you’re so lucky that you’re coming in right now, because they’re feeling unlucky because I’m telling them they have to have their tooth removed. But I spin it and say you’re so lucky that you came in now and we’re able to see this ahead of time. So you don’t do a root canal and then have problems, and then have it fail, and then have to take it out and do an implant. And when they look at it that way, they actually kind of walk out feeling a little lucky as well. So there’s that.
All right. So just to kind of finish up and tie everything together. Again I just want to go over the things that I find to be really important in creating a practice that is full-service for the community, full-service for patients, and where you can do your best work. So just take time, don’t rush, make sure you set up your schedule and your assistants and your office manager are onboard with the fact that you’re going to take a little time to get to know people, take a little time to ask questions, and that you’re going to really provide excellent care. Whenever I hear people talk about well I only had this amount of time to do it so this is what it ended up with, I just cringe at that. Because we really have as much time as we want and as much time as we need for each case. So make sure to take your time so that you’re providing excellent care.
Make sure you communicate with your restorative dentist for appropriately timing the sequence of treatment, whether it be again, restorative cases where you’re setting them up for the crown prep. Or if it’s something where before you even get started, needing to know what the restorative plan is, making sure there’s no surprises for anybody.
And then I just feel restorative is such an important complement to the endo practice. It’s something that a lot of endodontists will say there’s no way I can do that in my town, in my city. My referrals won’t let me do it. And I will say to that that it is something that you can start to do slowly over time. You start to do a few of these cases like what I showed you with the crown, and you call the referral and say hey, I really want to get all the caries out. My advanced irrigation system isn’t going to work properly if I don’t do it this way. And I’ll go ahead and get it set up for you so all you have to do is the crown prep. And hopefully they’ll say yes in a certain case, and then you do it once and then you may be asked to do it again a couple months later. You’re asked to do it again, and next thing you know they’re going to be asking you to do the restorative.
So let them kind of see how it can work for them as well. Or even take them to lunch and talk to them about it; that you want to start doing this for them and why. And that can be a great boon to your practice.
Treating kids can be very rewarding. It can be challenging for sure. But if we’re not doing it, who else is? I just really think that endodontists need to be treating kids and not just saying I won’t see anybody under 15 or 16 years old. Because the kids are oftentimes my favorite patients. They do really great and they can be actually easier than adults a lot of times.
And then my last thing is that I do think endodontists should be the ones doing endodontic surgery. I don’t mean that all endodontists need to be doing endodontic surgery, but if you’re an endodontist who doesn’t do surgery, I highly recommend you get to know a colleague – maybe it’s somebody that takes a call for you or you take a call for who does endodontic surgery. It’s only a few times maybe a year that you might see a case that really would benefit from surgery. And just make sure that you are referring to an endodontist who does microsurgery under a microscope and not pushing this off to the oral surgeons who don’t have the proper training or equipment to do the kind of surgery that we can do.
So with that, I will leave you. And thank you again for having me, and I really appreciate your time and attention. This is my contact information if you have any questions. And with that, I will sign off.
SEGMENT 2: Post-Presentation Discussion
All right. Well I thought that was an excellent presentation, very clear and organized. And I loved her topic, A Week in the Life, and seeing what represents a typical week in the life of an endodontist; filled with restorative issues, trauma, fractures, surgery, resorptions, etc. And I just think that’s a really great idea, because it’s so practical. She’s not showing her best ever cases. She’s showing what you can expect to encounter in an average week. And I think that’s just really practical and great for teaching, because it tells you what you can expect.
So for me, this makes her seem really humble and confident at the same time. Because I’m wondering all of you out there; how many of you would actually feel comfortable showing and explaining what you did last week. And maybe even those who said yes, might have hesitated. So what did you think of the presentation?
Well I liked so many things, but I liked the comment “full-service.” Because as a teacher for many decades, I can tell you. A lot of our clinicians don’t always flap the case and do the surgery; or they might do anteriors, but not posteriors. I see a lot of people – because we had a lot of endodontists come to Santa Barbara for training. A lot of them will back off on non-surgical retreatment a lot, and they’re just kind of into the clean/shape/pack game and diagnostics. So I like how she takes it all on, and I thought that was really good, the full-service.
And then I liked the – she said she wasn’t going to show her best cases; she was going to show like the consecutive cases – to her point, that’s what she did. But there were those seven images early that were like hero cases, and that’s where I picked up on that 3 Ps. You’ve got to have patience. If you want to do great work, you can’t be in a hurry. And she even reprimanded people at the end. Like she hears a lot of well, I just didn’t have time. Come on! Take charge of your life please. So patience.
And then of course you can have a lot of patience, but you better have perseverance, that’s my word. She said persistence. And then the third P was pre-curved; those small size, stainless steel hand files. And if you look at those cases that are on the screen when she drops those three words in, wow! Curvatures, loops, deltas. I mean you want to get that stuff, you’ve got to know how to instrument. So I liked that. I could go further. We’re going to do more of this later, but I did like how she just laid out. She did a resto case, and we just did pretreatment, right, just recently in a podcast.
When are you guys going to get signed up? You know, I have a lot of people coming in to RUDDLE+, but a lot of you are asking me questions that we talk about every damn time on RUDDLE+. Anyway, on RUDDLE+ we just talked about pre-treatment bands, copper bands, ortho bands, buildups. She did a great buildup and even talked to you, the audience, about how to encourage your general dentist to accept this so you don’t get into whose job is it, the things we like to feature on the show. So that’s probably an overview.
Okay. I also really liked what she said about communication. There were two things that really struck me. First she emphasized that you tailor your communication to who you’re speaking to. So she speaks to kids a little differently than she speaks to the special needs patient. Then she speaks to the woman who had no idea why she was there because she was asymptomatic. So I like that, that she makes her communication specific to that individual.
And I really liked, I thought it was genius how when she was talking to the male with the fractured root; how she said you are so lucky. And instead of focusing on or despairing about the crack, she pointed out to him that we caught this early and thank God we didn’t do all of this treatment only to have the tooth ultimately fail.
That was a really remarkable thing you just pointed out. How many times have we gotten involved in cases – now maybe not you young kids because you have CBCT, you have astronauts inside their bubbles, you’ve got all this stuff going on in your mind, you’ve got Star Wars. So you get involved, you disassemble a lot; you take teeth apart, it takes a lot of time. And all of a sudden it’s like ooh, can’t do it. So then you’ve to communicate that. But then the patient’s wasted time and money. The doctor, the endodontist, the principle has wasted time and money. And the referral is disappointed and maybe frustrated. So she really liked CBCT, so that was excellent and showed – we saw powerful examples where you wouldn’t have seen it with traditional films.
But then we were thinking, you and I were thinking about what would be another way we might pick that up, and that might have been with InnerView and Perimetrics. And I’ll just point this out. We’ve talked about it many times, we’re going to continue talking about it because it’s immanently coming to market. But when I was at the BU and gave that lecture that we talked about just earlier, on the second day, she had Dr. Cherilyn Sheets present. And she presented on qualitative percussion diagnostics, QPD. And that was Perimetrics’ InnerView.
So she does know about it, and she’s probably waiting patiently – impatiently on the sidelines until she can get her hands on it.
Yeah. Like one other show we did… Tough Question; Should You Remove The Crown or Work Through It? We actually had Dr. John West even weigh in and give his opinion on it. And she, Dr. Ferris-Wong said she really likes to remove the crown because it helps her see if there’s missed canals, it helps her see if there’s fractures. So yeah. I mean I guess if you use the InnerView and it seems like the restoration is solid and there’s no fracture detected, maybe it is okay to work through the crown then if you want to save the patient some money.
Sure. And in this case there was bone loss subcrestal, and it was coronal. So if you would have sent an electromagnetic percussive device against a tooth five times, and you get that oscillation, and then the feedback goes up to the cloud and then it goes into a database and it’s AI, you can begin to see how you’d pick that up. Because there wouldn’t be bone there, so the tooth is going to move and oscillate a little bit differently than if it had an intact PDL.
So yeah, really good stuff and it kind of brings us back around to it’s all interrelated isn’t it?
Yeah. So there was just a lot of great topics. Is there anything else that you wanted to talk about?
Is that a setup question? That’s a setup question. She had seven topics and I could talk five minutes on each one of them, at least. So yeah, there would be a lot more I could say, but I won’t. And maybe we can even use different formats and go back over to RUDDLE+ and the podcast.
Yeah. I think we’re going to do a podcast or a more in-depth discussion of her list of cases that she treated in a week. Because there’s just so many gems and learning opportunities in what she presented that we could actually talk about it at length. So we can actually do that on our next podcast.
So maybe just leave you with this comment; anything else I want to say. She said a lot that would not be fully explained in the time allotted, but the 3 Ps – let’s go back to those again. If you want to do cases and try to be like Cami (be like Michael Jordan). If you want to be like Terry Pannkuk, if you want to be like Steve Buchanan, John West, you’ve got to spend time, you’ve got to have a plan, you’ve got to have a lot of patience when it doesn’t go right. You can always reschedule – think on how she rescheduled. She could have finished, but no; reschedule – that costs money. Anyway, it wasn’t about the money, it was about the results. So I loved the 3 Ps and the pre-curved hand file.
Okay. I want to talk just a brief moment about legacy, because that’s what I do.
Oh, well she’s really on her legacy journey isn’t she?
Yes. And we actually talked about – the sports announcers that we talked about at the beginning of our show; they also have very powerful legacies.
Are they influencers then?
Yes. So Dr. Cami Ferris-Wong, she said that her mentor – the legendary Herb Schilder is her mentor. And she said that she feels like he is with her every day in her practice, even though he’s passed away. She hears things he used to say in her head all the time – it makes me think of Ruddle one-liners, we should do another segment on that – and it’s always inspiring her to be her best.
So I’m thinking that when you start out on your clinical journey, and you’re consciously or unconsciously embarking on creating your own legacy ultimately, that maybe the first thing you do is you just model yourself after your hero to start. So is that what you did?
Yeah. The old expression I didn’t know back then is “Model success; success leaves clues.” So it would be my -
Is that a Ruddle one-liner?
That would be my father, first of all. He taught me about hard work, integrity, honesty, helping people. And then I wasn’t very good at applying all that, but it was in there. It was inside me. So by the time I arrived at Harvard to go to Al Krakow – Alvin Arlen Krakow was my mentor and a second father. He was like – he would be fatherly to his residents and he was a fabulous storyteller. I learned so much endo with him sitting back. He had holes under his sleeves and he would tell a story that would go on and on and on, and we never tired of his stories. We would – almost like kids – beg for more. But anyway, what a great mentor he was. And then of course the great Herb Schilder. Al Krakow was Herb Schilder’s second student; I wonder if Herb Schilder influenced Al Krakow. Legacy, legacy, legacy.
So yeah, we’re all influenced by somebody so pick somebody that you really admire and respect. And you know what? Chances are you’ll be on your flight pattern.
It seems like it’s a good start to model yourself after someone you really admire. And then as time goes on, you kind of grow into your own role. So Dr. Ferris-Wong said a lot of nice things about you too, that you’ve influenced her in her career, so that was nice.
Well yeah. When I dropped by when she was that 18-year-old kid, I used to take her bubble gum.
Okay. All right. Well a big thank you to Dr. Ferris-Wong for that great presentation.
Thank you Cami, and we’ll see you up the line.
CLOSE: Unusual Ruddle Case Report
Okay, so in Dr. Cami Ferris-Wong’s presentation she showed cases that represented an average week for her. Now today to close the show, you’re going to show a case that is definitely not from an average week, right?
Nope, it’s not an average week.
All right, why don’t you show it and I’ll step aside.
Thank you. You know, it was interesting. John West does this. We saw an example, Cami Ferris does this, and maybe it is a Herb Schilder BU thing. He used to always say, show me your molars. Show me your last 10 consecutive molars. So this wasn’t a consecutive anything; it’s just a case that pops up during one of my weeks some years ago. I’m going to show some unusual cases that just popped into our offices. Ready? Here we go.
So these cases come into our offices. They have names attached to them, there’s histories. There’s some effort that’s gone into all these cases, but what they all have in common is they’re horribly failing. And that’s kind of been my normal fare in Santa Barbara for several decades.
Ironically, except for two of those cases – I told you wrong over there – but except for two of those cases, every one is retreated and has been successful and has long-term recall. So it might look pretty crazy to you when you get the unusual case, but step back and use your knowledge and your interdisciplinary ideas, and maybe get a couple other opinions and who knows?
So let’s focus on the last in which you’re going does not look unusual. In fact out of all the cases that scrolled by, this is the only one that you’re saying well, might be a younger patient. You can see the mixed dentition. We have a deciduous canine trying to exit. We have a permanent canine coming in. We have huge pulpal spaces. There was a history of trauma and the patient never followed up. It's a little kid, young kid. And who knows if it’s a communication issue; maybe the parents didn’t understand. But this is my pre-op.
So this little patient came in and they have a large, large, diffuse lesion. You can kind of see it down in through here. And you could even argue maybe more than one tooth is involved. But we got a normal limits to cold and a normal limits, and we tested canine to canine – not the deciduous tooth – and we saw thickened PDLs from the trauma that came in. It was a baseball. And we’re ready to go.
So it looks like it’s a pretty case, right? Pretty easy. The biggest thing is the communication; talking to the parents, another language. They’re Greek people so it was broken English, even with the parent. So Cami talked about communication, so sometimes it’s your hardest thing.
So I got the kid anesthetized; it was unremarkable, everything was going very well. I popped in through the lingual surface with my #2 round burr, surgical length, and bang! I hit a geyser. And we saw the drainage and my assistant and I are now sitting back and we’re patting the little kid, and we’re telling each other that with this geyser eruption, Panos was going to feel terrific tonight.
Well – listen carefully – oh geez. Guess what? We heard a big noise and a suction sound, and the clang of a clamp hitting a far wall. And we looked down, and we look immediately and there’s no rubber dam, there’s no clamp, and there’s no tooth! I’m looking right into the socket. So we start looking around. Oh! Guess what? It’s a tooth on the floor! So we have a tooth on the floor sequence. And we had to get another #9 clamp, because that other clamp was somewhere in the operatory, but it wasn’t the moment to find it. And I’m going to ask you; well, what you gonna do? Now what? Tooth on the floor, now what? I bet you didn’t train for that. So you can go back and read all your notes, you can look at all your old textbooks, you can go to the computer, and you can go online. And I bet you there’s nothing – I’ve got a special discussion here. Tooth on the floor, yes, it’s on page 47.
Well anyway, tooth on the floor means what? I think it means you have your ass on the line! The mom is sitting out there thinking Dr. Ruddle’s taking perfect care of my son; it’s a routine visit, he said it shouldn’t be too long. And little do we know, behind the scenes a lot of things are happening and they’re happening quite quickly.
So we took a shot. Yup, there’s nothing there; we should be able to replant the tooth. And we’ve all done replantations, right? At least Ruddle has. A lot of times people will come in with a tooth between their cheek and their teeth, or maybe they bring it in a cup or they have it in gauze. But this one was – talk about intentional replantation; this was an unintentional intentional replantation.
So it looks good; we can plant it back in. So that very same day we finished quickly by just replanting the tooth carefully. And then you can see the bonding in here, and you can see a little bonding – I’m pretty close to the screen, but a little bonding over here. I’ll get the lines out. And so we got it bonded together. Not a real solid bond; we want it to move a little bit. And with the tooth open so it can still continue to drain, we dismissed the patient with an open tooth that’s been replanted and it’s now bonded to the adjacent teeth.
I had him back while he was on the antibiotic, so it’s a 7-day regimen. I had him back about 2 or 3 days later and did a one visit. So start to finish, we went ahead and packed it; it dried beautifully. The tooth was snugger, but it’s still splinted so I can’t tell exactly what’s the splint holding it versus how much tightening. But you can already see in just a few weeks how much ossification can happen in these small kids. And basically you can see the lesion is getting greyer; not only internally, but its whole periphery is getting greyer. And you can see the bone is continuing to climb back in.
Did I mention on the pack, count the portals of exit. How many so we have? Let’s count them up. Okay, we’ve got 1,2,3; maybe we could say 3, maybe 4 POEs. Okay, that’s a good thing.
And you know I have to say this. There’s that guy in Boston, he can’t keep his mouth shut. He keeps talking about “The Look,” and there’s sexy lateral canals. He keeps talking about there’s sexy radiographs. You know what? Don’t get the lateral canals, but have fun.
So I’m having a lot of fun, and the last x-ray that comes up shows where we started way back just a few days ago, and this is like about – I don’t know, maybe two months. You can see this little canine is gone, so the canine is coming in so it’s a little later in time. But look at the magic of endodontics as a regenerative procedure.
So I hope you don’t have a tooth on the floor in your own office, but I do hope you know a little bit more about replanting teeth.
All right. Well thank you for showing that case. I notice that Dr. Ferris-Wong, she emphasized how much she likes seeing kids. And you can have this kind of fun if you see some kids.
You know what’s so great about kids? We’re treating adults all day so we’re very adult-like. But when you treat kids, you start to realize as you get older, you can be silly with these kids and they’ll be silly right back. And so you have a whole different atmosphere. So yeah.
All right. Well thank you for that and we hope you enjoyed the show. See you next time on The Ruddle Show.