Dentists are trained to thoroughly review medical and dental histories and perform comprehensive extraoral and intraoral examinations. Yet, in spite of these efforts to optimally serve patients, the dominant clinical reality is...
Endo, Perio & Surgery Endo vs. Perio & Posterior Surgical Access Challenges
The show begins with Ruddle & Lisette revealing their preferred toothpaste, because toothpaste is the superhero that fights the evil plaque villains! Then, can you readily distinguish between an endo problem and a perio problem? Ruddle and Lisette clear up the confusion in “Knowing the Difference.” After, Ruddle is at the Board focusing on posterior surgical access to the lingual root of a maxillary bicuspid. The episode concludes with Phyllis returning to tell us what she thinks about our Season 11 theme, Legacy.
Show Content & Timecodes
00:16 - INTRO: Preferred Toothpaste 04:45 - SEGMENT 1: Knowing the Difference – Endo vs. Perio Problems 34:44 - SEGMENT 2: Posterior Surgical Access Challenges 56:37 - CLOSE: What Does Phyllis Think? – LegacyExtra content referenced within show:
Other ‘Ruddle Show’ episodes/podcasts referenced within show:
This transcript is made available by The Ruddle Show in an effort to share opinions and information, and as an added service. Since all show text has been transcribed by a third party, grammatical errors and/or misspellings may occur. As such, we encourage you to listen/watch the show whenever possible and use the transcript for your own general, personal information. Any reproduction of show content (visual, audio or written) is strictly forbidden.
INTRO: Preferred Toothpaste
Welcome to the Ruddle Show. I’m Lisette and this is my dad, Cliff Ruddle.
How are you doing today?
I’m doing pretty good. What about you?
I thought you enjoyed the Olympics.
I did.
Okay. Well excellent. I’m really excited to have all of you here, and we have a pretty good show going. It’s a topic that’s riveting in the first segment.
Okay. I don’t know about all of you, but I’ve often wondered if the toothpaste that they had out at the dentist’s office is actually the toothpaste that the dentist uses at home. So there are so many toothpastes out there, and not necessarily a lot of different brands of toothpaste, but every toothpaste brand has several versions. So there’s the fluoride toothpaste, the whitening toothpaste, the ones that control tartar, promote gum health, strengthen enamel, freshen breath -- just a lot of choices. And we’re not going to compare and contrast toothpastes today. We’re just going to tell what we use and why we use it. So what toothpaste do you use, and why?
I have no reason for any toothpaste that I use except it is arriving at the sink in the bathroom and it’s Colgate. And your mother chose Colgate. I think she chose it because she is very analytic. I looked it up and asked her more about it, and she said that it used to come in a jar in 1873. This was just barely before. And then she waited just another few years, about 17 years, and she loved it because it went into a tube. So she likes Colgate; we buy Colgate. Crest is number one, Colgate’s number two.
I don’t know about Crest, but I know Colgate. I’ve seen a lot of Colgate ads, really old ads, like turn of the century, 1900. So I used to use Colgate because that’s what Mom uses. But then I now use Arm & Hammer Complete Care, which is a baking soda toothpaste. I just kind of like the idea of a baking soda toothpaste. Apparently according to their website it removes three times more plaque, neutralizes acid, is less abrasive and whitens more gently. So how accurate this information is, I don’t know. But I’m pretty satisfied with my toothpaste, as you seem to be with yours.
Well the audience might know that toothpaste formulations haven’t really changed in 60 years. I read that. You can Google it. But they’ve really worked on marketing and they’ve really worked on the tube construction. So if you’re into R&D, when you squeeze that toothpaste it has to come out a certain way and there’s been a lot of effort in recent decades to get that squeeze just right.
Okay, well I don’t know if anyone’s going to be changing their toothpaste based on this segment, but just keep brushing so you can keep smiling, right?
Well today we have a great show and let’s get to it.
But I had a joke!
Oh, okay. You have a toothpaste joke?
Yeah. Why did the toothpaste tube break up dental floss?
Why?
Because it didn’t want to have a relationship with any strings attached.
Okay. Way to set the mood for this show! So let’s get to it.
SEGMENT 1: Knowing the Difference – Endo vs. Perio Problems
Okay, so it’s time for another segment of Knowing the Difference. And this favorite segment of ours is inspired by a quote by the 18th century French author, Madame De Stael, who said: “Wit consists of knowing the resemblance of things that differ and the difference of things that are alike.”
So with that in mind, we’re going to discuss the critical distinction between an endodontic problem and a periodontal problem. And in some cases, you may be dealing with both an endo and a perio problem. So when the etiology is uncertain and you’re looking to refer, you might not know if you should refer to an endodontist of a periodontist. So today we’re going to talk about some criteria to consider when making a diagnosis, as well as talk about how to best proceed in cases of uncertainty. So why don’t you first tell our viewers how dominant an issue this has been in dentistry over the years?
It’s the most dominant thing you’ll ever experience in your life. No, to your point it’s received a tremendous amount of international attention. I mean I’m talking about over 50 – 60 years and that’s just more of less my time – 50 years. But it goes back; you can go 10-15 years before that. So you find many – almost any earnest endodontic textbook has chapters -- a complete chapter dedicated to the inter relationships between endo and perio. Peer review journals have pounded on it; rag magazines have never ceased to publish these kinds of articles. And then of course there’s a lot of case reports. So altogether, there’s been a lot of interest because it’s a dilemma. And we’re going to try to make it a little easier today, and we can make a lot of them easy.
Okay, easy. I guess in a year, I would say it’s a real dilemma about zero times out of 100. But behind that expression, it can be a dilemma. And I’ll tell – we’ll talk about this later when we talk with other specialists. Sometimes it’s hard to flush it out and what we do.
So anyway yeah, it has been a dilemma for a long, long time. And how do you handle that dilemma? Of course I’m an endodontist; why don’t we just do the endodontic examination? It all starts with what we’ve talked about and pounded and pounded in RUDDLE+, on the Ruddle Shows, podcasts, diagnostics, clinical findings, pulp testing, radiology, could be tomosynthesis, could be CBCT, could be your three well-angulated x-rays.
So that’s kind of an overview. If you want to get to the big dilemma, learn to be a magnificent endodontic diagnostician.
Okay. We’ll talk about those things as we go through the critical findings, the pulpal sensibility testing, and the radiology. So we’re going to get to it all.
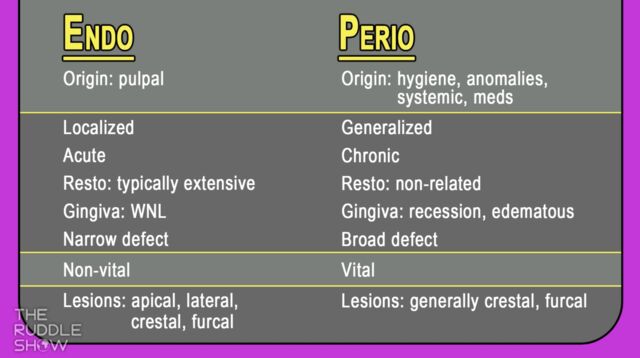
All right. Let’s bring up our comparison graphic and get started on noting some similarities and differences. So at the top of the list we have – I see that the etiology of endodontic problems differs from that of a perio problem. So maybe you can explain this a little more.
Okay, I’d be happy to. These are like landmark, black and white. So over here boom; over here boom. Well of course it’s never quite that clean. But in general, if we look at the table, the origin obviously of endo problems is pulpal. It’s pulpal. And we could talk about trauma, orthodontic tooth movement. When I say trauma, I mean crown prep. I mean placing a Class 1. I mean taking out a Class 1 and going over the marginal ridge and now it’s a Class 2, Class 5 buccal. So I’m talking about trauma from our work, trauma from orthodontics, trauma from out in the streets – basketball, sports injuries, pulpal.
Usually when we see toothaches we’re talking about inflammation and infection. So let me just set off a tome here -- endo/perio. We’re trying to find out is it the inflammation that comes first and then the infection; is it one or the other? So endo is more localized; it’s more like it’s right here. Perio, a lot of times it can be localized and that already defeats the table. But in general, perio as we all think of it is a generalized problem. The upper right quadrant is about the same as the lower left, upper left, lower right, so it’s a generalized condition.
Toothaches are usually acute. They come in and they didn’t sleep well last night, actually didn’t sleep much at all, then I came and saw you. Perio: I’ve seen acute ones. So again I’m defeating the table a little bit. But generally they don’t hurt. People come in and say it bleeds, it’s sore, my tooth seems loose, I have a bad taste in my mouth. But anyway, it’s more chronic, it’s not so acute; but of course we’ve all seen a periodontal abscess haven’t we?
What else do I have? We’re going to go into a lot of these in more detail, but usually restorations, endodontically treated teeth; again bear in mind the table is just real quick, is it this or that? But I’ve seen, you’ve seen, we all have seen virgin teeth endodontically involved; they’re cracked. We’ve seen minimal restorations seemingly miles away from the pulp chamber; pulp’s involved. But generally they’re heavily restored. So in general, endodontics – heavily restored; perio – it’s not so much restorative related.
So let’s just go down that far now, because we’re going to come back and beat some of this to death.
Well why don’t you talk about what are the etiologies of periodontal problems?
Well that’s good. When I said perio I said it was so simple didn’t I? It’s usually hygiene related, so the biggest – if it’s a pie and you’re sectioning off what proportion to assign to hygiene, that would be by far the biggest piece of the pie; hygiene. Tartar, plaques, calculus, stuff like that. But there are some things that we know that we should be more aware of. How about anomalies? If you have an ectopic enamel layering somewhere around the crown of a tooth, that’s called an enamel pearl. How many times have we seen periodontists have to find a narrow defect, or a kind of a broad defect, oozing gum, edentulous tissue; and they pull it back and there’s an enamel pearl that they have to shave back or shave off? So anomalies like fractures, supernumerary teeth. Some incomplete fractures are just subgingival; they’ll raise hell with the soft tissue and it’ll be quite sore and bleeding.
So that’s sort of your anomalies, the enamel pearl I mentioned. But then there’s also systemic diseases. How about osteoporosis? We see oral manifestations. So we’re talking about systemic diseases with oral manifestations. So we see osteoporosis, chronic liver disease, gastroesophageal reflux disease – GERD, all caps, G-E-R-D. So there’s lots. Vitamin deficiencies, a lot of hepatitis; lots of hepatitis out there, A,B,C. Well if it’s not controlled, we see oral manifestations.
But by and large I want you to look for meds too, because if you see these systemic diseases on your medical histories, look at them; ask exploratory questions, delve deeper. You might find out that some of these people, largely women, they’ll be on like bisphosphonates. And bisphosphonates are to treat Paget’s Disease, osteoporosis; but we see medical related osteonecrosis of the jaw so it can be rampant.
So that would be sort of a little umbrella over the hygiene, anomalies, systemic disease and medications.
All right. Well just looking at our graphic -
Was that beautifully done?
Yes. And you touched on a lot of the clinical findings. I know that you were also emphasizing it’s not often just one or the other. Sometimes there’s a grey area where you’re trying to determine what could be the cause. I see on the list that an endo problem is generally more localized, but you also said that a periodontal problem can be localized. So maybe talk more about when you’re doing your clinical findings, what you’re looking for to help you make the diagnosis.
Well what we’re both missing, and you know it and we know it, but I’ll just say it. We’re going to get to it: vital pulp testing. But right now, when you probe around an endodontically involved tooth, it’s been my experience that by and large, it’s the soft tissue; the attachment apparatus is within normal limits – WNL.
But there’s exceptions. We can have narrow defects sometimes secondary to either a portal of exit of a necrotic tooth, or we could have a fracture that extends sub-G and subcrestal. And so the gum pulls away, the bone pulls away, and a narrow defect.
In perio, unlike usually in those normal limits, soft attachment apparatus is okay. In perio, the tissue is edematous, it bleeds, it’s puffy, it’s kind of got a glassy sheen on it. And you can probe along, 2-3, 3-4, 4-5, 5-6, 6-7, 7-6, 6-5, 5-4. So they’re crater lesions. You step down and you step out of them. They’re broad lesions; they’re not narrow. So those are distinctions. So clinically with the examination – we’ll get to the pulp testing – but I want to know if the crown even is causing any of these problems. But yeah, pretty much no defects with endo, or they’re very narrow which is classic. Perio is broad, cratered.
Could the occlusion like on a restoration cause periodontal problems? Or is that – I mean is the occlusion ever an issue?
It absolutely is, and I was going to talk about that in a little bit. But if you’re pounding on a tooth, or you’re going into – we’re talking gnathology– you’re going into work and balance and maybe protrusion. If you’re tripping over a cusp or you have a plunger cusp up above, to her point, you could actually – not so much because you’re beating on the tooth, have the bone pull away – but you could crack the tooth. And secondary to a crack propagation, we start to see pockets.
All right. Well so we’re going to have this graphic in our show notes, so you can refer back to it. But we kind of touched on the clinical findings which is in this second area. And now let’s go to the pulpal sensibility testing, because I understand this can be helpful too when making a diagnosis.
Pulp testing. You’ve got to get really good at it. I know for most of you out there, because I’ve been around a long time; I talk to you, you come to classes, we communicate over the internet, I travel millions of miles. So I know how you’re thinking by and large. So you’re thinking, you know I do pretty good pulp testing. Besides, I can almost always identify the chief complaint. Patient’s coming in, is it endo or perio, you can usually get to the truth. But if you could just even get better.
So first off I’m going to say let’s get a baseline. Because you don’t want to fool the patient and you don’t want them to fool you. And they’re hurting, so they’re a little anxious, right? So you just can’t come at them with a piece of ice and then you might get an exaggerated response and now you’re making the wrong diagnosis.
So let’s get a baseline. If the problem is down in Ruddle’s lower right quadrant, start on the lower left quadrant. Do a little bit of pulp testing up here. Catch a few anterior maxillary teeth. And get used to hand signals: raise your hand when you first feel the sensation of cold in your tooth. Check! Keep your hand up as long as the sensation lingers, and when it goes away, lower your hand. They didn’t hear a thing you said. So by the time you get them into the hand signals and you do two or three teeth, you’re starting to get them used to the test. And as they become used to the test, you’re going to get pretty reliable information.
I’ll throw in – we haven’t gotten to radiographs yet, so you’ve got to marry this whole chart area with the whole picture. But obviously if the pulp is receded, if it has sclerosed and mineralized in, and if the crown portion is a block of dentin, they will not feel hot or cold. So you can think oh, it’s a necrotic tooth; let’s rush in and do endo.
So hand signals and baseline is what I’m starting with, and then of course generally I do a hot or a cold test. If I ask the patient are you having any problems with cold. I never say them together. I never say are you having problems with hot and cold. They’ll say yes and you don’t know which one. So I always say are you having problems with cold. If they say yeah, like it kind of zings over there and it lingers a little bit when I swallow; I’m running a cold test. If they say no, I haven’t noticed it hurts to cold; then I might ask them coffee, tea, is all that good? Yeah. Well then I’ll run a cold test; it’s easier. But if they say it hurts to heat, I’m running heat; if they say it hurts to cold, I’m running cold. Reproduce the chief complaint.
So you’re looking for what? The immediacy, the intensity, and the duration. That’s what you’re looking for. Baseline, hand signals, immediacy, intensity and duration. And when you start to do that, you’ll start to separate out pulpal problems and etiology and origin from lesions of periodontal origin, LPOs.
And I guess it’s important to do the whole mouth like you were saying, get a baseline. Because maybe all of their teeth are very sensitive to cold.
Yes. And let me just say what the audience knows. They need to know what I know; Ruddle knows. People that have a lot of periodontal disease usually have recession. They have infrabony pockets. They have exposed cementum. And oftentimes just one single cleaning by the hygienist in the cementum layers, it’s gone, it’s only .7 of 1mm in the crestal coronal one-third. So one root cleaning procedure eliminates the cementum, and what’s under the cementum? Tubular dentin. And now there’s direct communication to the pulp. So when you put cold on those teeth, they will feel it immediately. Intense – they’ll say it’s a 10 or 11 on a scale of zero to 10. But it goes right away. So if it goes right away, that’s probably an inflamed pulp, but probably the etiology is over here in perio. It’s an LPO.
Okay. Let’s move on to radiographs, or CBCT images. I just want to ask you though, that just noting a lesion on the radiograph doesn’t necessarily mean it’s a lesion of endodontic origin. There’s periodontal lesions as well?
Yeah. In fact we were talking about this several times recently. You tell me; where can I find a perio lesion?
Well it says generally crestal or furcal.
Well you’re reading perfectly. That’s it, we know that. I mean nobody is looking around the apex of a tooth to identify an LPO, lesion of periodontal origin. So it’s just like Lisette said; they’re high, they’re around the crown, they’re crestal. But the thing is we have – molars have three roots; we can have trifurcation involvement. Lower molars have two roots; bifurcation involvements. When I said supernumerary tooth, I didn’t even mention radix intermolaris, radix paramolaris. Sometimes these anomalies cause perio defects, so that’s why we were talking about all those anomalies.
So you’re right. The lesions are dominantly crestal or in the bi and trifurcations of multi-rooted teeth. Whereas endodontics, the lesions are – okay, they’re dominantly apical, so let’s make the table work a little bit for you. But the folly of a table – this is our table. But if you pan and go on the net, if you open up 10 textbooks, you’ll find a similar table. A little different tables. The point is it’s never this or that. So that’s why we’re saying there’s – we should have had one down the middle, question mark. Because one goes this way a little bit, one goes this way, and you’re going is here, is it over there, or do they meet up in the middle?
Endo is classical apical. The portal of exit that you all put your files to and go to the end, we talk about patency. That’s usually where you’ll see on non-endodontically involved – I mean endodontically involved teeth, but non-treated. You’ll find apical lesions, you’ll find asymmetrical lesions that crawl around the root. You’ll find lateral root lesions, nothing apical; or maybe apical and lateral. And Ruddle has found many furcal canals after obturation. I have found many crestal defects that the bone rises back to the surface. Just like Herb said when I listened to his endo/perio lecture back in the mid-70s.
So you’ve got to kind of be aware of – okay; you’ve mentioned up something about “it’s the anatomy, stupid.” You were talking to me, not you. She said it’s the anatomy, stupid. She was talking to me.
I was talking as if you would say that.
Well I might. But the point is it was a brilliant comment, because here’s what I’m going to say off of that comment. If you aren’t seeing many portals of exit filled on post-operative films, then you’re not going to probably make the connection between a crestal defect that’s a LEO, an endodontic, or a furcal canal that’s a LEO in etiology, in origin. If you’re not seeing those filled on your routine films, then you’re thinking all those up there high around the crown are probably lesions of periodontal origin. So it really is about the anatomy. And I keep pounding this guy, but I do love him, and sometime we’re going to actually do something together; he just doesn’t know it yet. I’ll tell Ollie when it’s time. Okay Ollie, wait and be patient. It’s not sexy lateral canals, it’s portals of exit. They just happen to be sometimes in the crotch of teeth, sometimes in the coronal one-third, and they have – then we see lesions that are attributed to periodontal disease. They’re masquerading around as lesions of periodontal origin, and in fact the etiology is endodontics.
Okay, well I have a couple of comments.
Did that answer what we were supposed to be doing?
Yeah. I just have a couple comments, and one is a little bit off what we’ve talked about. But the first thing I wanted to mention is it’s become clear from our discussions today that often it’s a combination of both. However, I would like to say that I have seen cases you’ve treated, radiographs of cases where the recall shows healing. And the periodontal problem, if there was one, also seems to resolve itself when the endodontics is done.
Now I’m thinking this doesn’t work the other way. Like you can’t – if it’s a combination of both, you can’t just focus on the periodontal problem and the endodontic problem will resolve itself. It usually doesn’t work that way; that’s my first comment. And then my second comment is sort of connected. If you’re a general dentist and you think it’s a combination of both problems, who do you refer to first? Or do you refer to both?
I typically drop on my periodontal knees. No, I mean my endodontic knees. Oh no, I have two knees: endo/perio knees. I drop on my knees and pray to the gods. No. It’s very normal what she just said. It’s so normal that that is how you have to approach these things.
So in every community – okay, not every community. But in most communities in modern countries, you’ll have in cities, in populated areas, you’ll have combinations of specialties. You won’t have every specialty, but usually a community has a periodontist; usually a community has an orthodontist, and usually they have an oral surgeon, and they might have a – okay, they have some specialties. I like to find people that – I’m talking about periodontists – that are knowledgeable; they have to have knowledge. That means you probably have to have experience to have knowledge, because you can have knowledge and no experience, but if you have experience it shapes knowledge. So I like knowledgeable, I like experience, and how about the word “trust.”
So we had a lot of really great people, three or four in Santa Barbara I worked with routinely. I started out with Nells Johansen. But the one that I ended up working with the most was Richard Sanders – rest in peace, Dick. Richard and I worked together for decades, and the connection was he went to BU. So he went to Boston University, Goldman School of Graduate Dentistry. He specialized in periodontics. But guess what he learned when he was at BU? He had to go over to the endo department and take endo classes from Herb Schilder. So he knew all about root canal system anatomy, he knew all about portals of exit, and he knew – listen carefully – he knew the lesions form adjacent to the portals of exit. So when he saw a furcal problem, he wondered if there was a portal of exit from endodontics from a necrotic tooth that was feeding it.
So I don’t know if I said this yet, but I better come back – we were talking about pulp testing. It’s a slam dunk if you put ice on a tooth and there’s no response and it isn’t calcified, do the endo. Because it’s a necrotic tooth. It’s got to be doing something and it might be your salvation; it might solve everything.
So Dick didn’t like pulps. He said he never met a pulp he liked. So he said pulps – he actually said to me when I was very young: “Pulps aren’t sacred, get it out”! So if it needed to be done because it was necrotic – let’s make another signal – couldn’t we put ice on the tooth and it’s vital, it’s severe, they hand goes up, it lingers, you’re looking at your watch, it’s been a minute and their hand’s still up and they’re like this. That’s a bad pulp!
So they can be highly inflamed and contributing to lesions of periodontal origin; or they can be totally necrotic. So I want to come back and explain that from the vital pulp testing, but Dick wanted me to do endo first. So if the endo just needed to be done, nobody told me, I just did it. Okay, it needed to be done. But what was left was not now endo. So the whole key here is sometimes you do endo, not promiscuously, but to rule it out. So it’s not part of the diagnostic pathway or decision tree.
Dick said whatever’s left, send it back to me and we’ll go from there. What did that mean? Apically repositioned, flat, what could be just hygiene. Because a lot of times after endo things did improve, but maybe not completely. Maybe it was so chronic it never had time to heal, and now it can’t heal because too much saliva and debris and plaque got down there. So it might just be hygiene; follow-up. It could be apically repositioned flaps and osseous recontouring. It could be hemi-section and a root amp in that era. And it could have been an extraction and an implant.
Okay. With what I’m hearing from what you just said is that you had a lot of trust for Dr. Sanders and his work, and vice versa. Because it wouldn’t make sense to say let’s rule out the endo problem and send it to an endodontist who then does shoddy treatment, and then you have even a bigger problem than you started with. So you really need to be in a relationship with someone you trust and you know their work.
Yeah, and you had this in the script and I failed to mention it. Because there’s so much to talk about; I mean that’s why there has been chapters. When we talked about radiographs, I didn’t mention the instance where it has had previous endodontic treatment. Could be looking fine. I know, ha-ha; we can judge on an x-ray the quality of the endodontics. Really? Not completely, but you can see if it's short, you can see if it’s long, if they missed a canal. There’s so much that can be learned from a well-angulated post-operative film. So my pre-operative film could be revealing previous endodontics, like she mentioned in the script. And if you have a lousy root canal, redo it! Because there might be a portal of exit that just boom; a rope of gutta-percha sealer right out to an infrabony pocket, and it’s a round of applause.
We’re going to bring this home for the audience in much better specificity than the script. This is a fly over. This is because so many dentists talk about this stuff. But we really need to show several cases, and I don’t – we’re not going to do that today. I’m going to show some pre-ops only.
Why don’t you show – do you have a collage of cases? Because I had mentioned that a lot of times when you do the endodontics, the periodontal issue gets resolved.
Right.
So maybe.
I guess I’ll turn my chair a little bit so I can – you know I failed. Hereditarily I didn’t get the third eye in the back of my head like some did. Every one of these cases was treated successfully. All roots but one were retained. If you look at the left upper image, it’s a posterior bridge abutment. It has a deep infrabony pocket. Lisa was pointing it out, I asked her where’s the perio lesions? They’re more crestal. Well it turned out that that was a really broad defect and the situation was hemi-sect, save the mesial root so we have a new bridge abutment. Today you might say implants dummy. You know what? I’ll show this later; we have like 20 years on it.
So before you jump to some of these “newer,” so-called more innovative procedures, don’t give up on roots. You know, the naturally retained root is the ultimate dental implant; when endodontics is properly performed.
Middle. This person’s been going to a hygienist for a long time. It’s the molar, it’s the first molar. You can see a gouge in the distal aspect just under the margin of the crown. That’s where the Gracey (curettes) have been going. There was a massive lateral canal that was uncovered. The patient exacerbated and blew up clinically secondary to a cleaning. So there is communication, endo/perio.
We’ll go quickly. The far right one, upper, G-shaped lesions, apexed it. Those by many of you, you think those are cracked roots. I have that completely healed; I have a 30-year recall. Endo/perio, pulp testing, clinical findings, radiology, what do you do here? Bottom image on the left. Where’s the lesion? Not so apically is it; it’s distal crestally. There’s a rope of material that’s going to go right out there from a necrotic pulp.
And then our last case – this is an old case; I’ve shown this all over the world – but it’s a case I showed at ProTaper Next I think, when I was talking about ProTaper Next for about five minutes in that era. Where’s the lesion? You might say thickened PDLs around the apices Cliff -- maybe the mesial, maybe the distal. Seems to be sitting down the neurovascular bundle. But what about the furcal canal? How about the furcal lesion?
So radiology is critically essentially. You’ve got to put together the clinical findings. I’ll go back to loose crowns, didn’t even mention this. We just said the quality of the crown; does it fit, does it not fit? It’s not that simple. Have them bite on a stick. What if you see bubbles emanating? Every time they bite, bubbles emanate. That’s a loose crown, that causes periodontal problems, okay; something just like that. Fractures, loose crowns, coronal fracture under the crown. I mean there’s a little movement. Is it the tooth that’s moving or is it the crown that’s moving independent of the tooth?
So lots of stuff that it’s hard to do in just 15-20 minutes, but that’s a pretty good overview and touching the surface of all the things you should be thinking about.
Okay. Well thank you for all the information and the collage. Like he said, he does have – he had isolated originally three cases to show case reports for three different cases for this segment, but it became clear that this was going to be too much material. So we will do more on this in an upcoming podcast.
In fact I’ll interrupt you. I was going to show every one of these all the way to completion, and you know what? That was like another 30 or 40 minutes. So she said oh no, not so fast Charlie. Cut it back. So I cut it back to three unrelated cases. Just to show the concepts, but unrelated so you wouldn’t see these until later. Those got pulled too. So this is a good discussion with a little bit of eye candy. But we’ll come back and we’ll take it on.
Okay. Well thank you and that’s all we have time for right now. But we’ll move on to – I forget what’s next. But anyway, we’ll go into our next segment.
You mean what Phyllis thinks?
Yeah, but I’m not sure.
Oh, I have a big surgery! I’m going to scrub in; I’ll be in my scrubs and then we’ll get Phyllis out here. I understand.
There is something that will be following this segment.
SEGMENT 2: Posterior Surgical Access Challenges
Okay. So here we are with another session At The Board. I’m really happy to see all of you out there. Now today’s going to be a topic – it’s going to be just a little narrow focus on lingual root, the palatal root of maxillary bicuspids. Usually that would be the first bicuspids. So the reason I’m doing this is because I have gotten some conversations from you out there, especially some of you RUDDLE+ people, and you’re going when are you going to talk about that lingual root? It’s so far into the palatal we thought it was harder than the palatal root of a maxillary molar.
So I want to just have a brief interruption of what I really normally wanted to do, and just give you a little heads-up on that area so some of you can be more comfortable when you’re assessing maxillary first bicuspids for surgery.
All right. I want to thank you for joining us again, and I want to thank you for all the activities and questions that are coming in. A lot of you are signing up and you’re getting baptized regarding surgery. We have these big continuums, as you know, and we’re not releasing intentionally everything at once. Because by the time we get to the end, I might even have to go back and edit something if conditions on the ground change.
But just understand that we’re releasing at a cadence. We’re about a dozen in on surgery, and we have to get to almost 30. So there’s a lot of content that lies just ahead. Let’s get started.
All right. So the palatal root, the lingual root; it’s the same difference. But let’s look at the challenges. When you assess this tooth, I think you would immediately think we’re not doing retreatment because there’s too many violations of the cleaning and shaping objectives. The mechanical objectives, we can just rattle them off real quick; we’ll reduce it to four. Look at any canal and ask yourself, is there a continuous, tapering preparation?
Maybe we should do it a little bit different. Maybe we should look at the other angle and come even more mesial so you can see those canals more in their entirety. So do we have a continuous tapering preparation? That’s a yes or no; you’re the clinician, you’re assessing, retreatment or surgery.
Did we maintain the original anatomy? It’s hard to imagine; you could have all this going on up here and that foramen was kept really nice and tight in its physiologic dimensions. Did we maintain the position of the foramen on the external root surface, and did we keep the foramen as small as practical? So when you start to click through these objectives, you start to realize we have no chance of retaining this. In fact, I’m going to come back and say I’m not showing you intentionally; I had the third angle.
We always want to get three horizontally angulated films. We can come straight on, break the contact areas, we can do that. We see the cull; you can see the cull area in here, you can do all that. But when we start to move the cone more anterior, we get to see that buccal root moving off towards the posterior. And that frees it up so you can really assess.
Now you might have liked your – the lingual root, continuous tapering preparation, the original anatomy, maintain the original anatomy, maintain the position of the foramen maybe, and keep it as small as practical. As small as practical; I didn’t say possible, I said practical. Maybe -- maybe on the lingual; maybe on the lingual. But not so much on the buccal. On the buccal we have a lot of violations of the mechanical objectives.
The more mesially angulated film also starts to throw the roots around, and it starts to give you a sense of what lies ahead. In other words – look at my fingers – are the roots like this? This is your x-ray, right? You say well I don’t see barely one root, but maybe I see now two. Are the roots in a proximal view like this? Or is there significant splay? Is there significant splay where these roots are really being thrown further and further apart, in mesially, progressively angulated films? So get one and then come mesial to mesial; okay?
And as long as you’re using your aiming devices, your Rinn kit devices, you’re going to get pretty good images, one-to-one, but it’ll help you diagnostically. The endodontists are screaming; they’re yelling Cliff – CBCT! Well you don’t all have CBCT, but if you had that, yes; if you have tomosynthesis, check that box as well. Look at image stacks like we’ve talked about in previous shows.
So you begin to plan your surgery because you realize you can throw these roots quite a bit apart and you know the distance. You’re going to raise a flap up; you’re going to lift this flap up and free it up here. And then you’re going to make your access and you’re going to come through here, and you’re going to have to take a lot of that buccal root off. You’re going to have to lose at least about one-third of the overall length.
So this brings us back to periodontal probing, mobility, crown/root ratios, is this the best treatment approach, should we do an implant, could we do a bridge, what should we do? So if you start to think like that you’ll have the right answer.
So understand then about one-third, the apical one-third of that buccal root is going to be gone, because you need access, access, access. It’s just like occlusal access. You can make a really small ninja access, okay? Can you find all the orifices, can you visualize the axial walls, can you see fractures? If you can do all that, you can make them as small as you like.
And then of course that’ll get us on over to the lingual root, the palatal root. So I’m referring to this as lingual or palatal, for international guests the same thing, same difference. But we’re going to have to get to that root as well.
So with all your imaging, whether it be CBCT, tomosynthesis, conventional radiographs, three different horizontally angulated films; get them. And treatment plan for no surprises, how about that?
Okay. Now that we have that out of the way, let’s come back to the case and show it. So when I made the flap and lifted the flap up, you immediately see – we’re looking at about right in here; right in here. The gutta-percha is leaving the root laterally, and it has perforated laterally, and the apical extent of the cone is lying right up over the root. So it’s superimposed over the root, and I’m pretty close to the board, but you might say it actually looks like it’s inside the root. Maybe in some dimension. So you might have been a little fooled on that; CBCT would have plucked that right off. But remember, that just has come on really strong in the last 10 years, 15 years, and it only arrived in the United States in 2001. So it’s still, we would say, relatively new technology about a quarter of a century in. Because so few of you have it.
All right. So that is a perforated root, so we’ll start to work on that. And as we knock that root down, as we knock that root down, just like we said, it’s nice and flat, it’s been almost a zero-degree bevel, and you can see it probably – I’m again close to the board, but maybe you can sort of see it if I go like that. And you might even see the foramen right in there. So all that to get across to see the apical one-third, to see the big old dome-shaped palatal root from the buccal view, and to get a good visualization.
So go ahead and begin to knock that down so the apisection continues so you have nice flat tables. You can use methylene blue and dye, make sure you’re around the root and you can read PDL; the dye will be absorbed into the periodontal ligament space. And I’m using, back in that day, one of the first ones in the world, we were using coated surgical ultrasonic instruments. Thank you Gary Carr for getting the concept going. You didn’t do the coated part and the contra angle part, but you certainly gave us the root end preparation idea. Then others came behind and made the instruments even better and more efficient. And less wedging because we could cut with easier motions with a coated instrument.
So we also had tips that were 3mm long, and we had tips that were 5mm long. So we could go further up the long axis, but then you had to have enough room in here to introduce the instrument. So you might have to start with a 3, and that would be a little smaller profile; and then once you get that prepped out down in deep, then you can come in with a 5. And a 5 might be able to not quite hit here, and I’m not saying remove more bone; I’m just saying you can start to usher it into the prep and then stand up your handpiece and you’ll be able to go 5. So that’s just a little idea.
And so very quickly we’ll walk through it. There’s the two roots; you can see they’re stair-stepped just like we showed. Look at all this height in here; we’re saving that root. A lot of times I see clinicians knock the roots down so they’re kind of on the same plane, but you’re going to really shorten the stability of that tooth by shortening – by needlessly shortening the lingual palatal root. So that’s that dimension, you can see it right there.
I pride myself in photography. It wasn’t so easy, and a lot of these were done before video was even remotely good. And certainly you couldn’t get grabs off of video to have a really sharp resolution; an image with a good resolution. So that’s our retro preps, and you can see them quite nicely. But to really look up the prep, and to really evaluate; do you have gutta-percha left on your axial walls of the prep? Is there any debris residual to the prep? Are you on the long axis, or did you get a little bit deviant? This is a way with these tiny retro mirrors that we talked about decades ago. And in the surgical symposium on RUDDLE+, you can see a lot of things we did with the mirrors and how we used them in a lot of just routine, bread and butter surgeries. But to me, I love to evaluate. A lot of people prep, but come out, and it’s a blind shot to go right on and fill. Why not evaluate it? Why not evaluate it?
And why not even use the little mirrors to look at your seal? Whether you used MTA, whether you’re using amalgam, super EBA, whether you’re using some kind of a bio ceramic putty. Okay, that’s fine, that’s all good. Whatever you’re using, evaluate the cork.
So we started with that. We’ve shortened those roots down as you just saw surgically; got quite a bit more height up here on this root as compared to the buccal root. And you can begin to see if you watch with time, the bone comes back in. Endodontics properly performed is a regenerative procedure; it sets the stage for ossification, bone growth, reattachment, and that’s what makes endodontics the foundation of restorative and reconstructive dentistry.
So that’s just one case, and now we’ll move very quickly because I showed you kind of the nuts and bolts. Now you’ll need to go to RUDDLE+ is you want to know all the things about flaps, elevations, crypt control, hemostasis, apicoectomy, retro preps, suturing. Okay, all that’s somewhere else. This was just I’ve had some issues lately with people calling and saying oh that lingual root’s deep. You know what? It is deep. It’s one of the hardest surgeries in the mouth. The palatal root of the molars, the lingual or palatal root of the first bicuspids. And of course there’s some issues down below; mandibular canal, middle foramen, and then the inclination of incisors. All of that’s discussed in another venue and in more content.
So now that you’ve see this, and I’m so close to the board today for some reason, I can’t see my own work. But this was done recently by and endodontist in southern California, within six months. They’ve been on an antibiotic post treatment. This tooth was percussion positive and palpation positive. But if we apply that to this tooth over here, this one, it was percussion – boom, boom, boom. In other words you couldn’t even touch the tooth. That tooth was very, very sore in palpation; there might have even been a little fullness up in the vestibule. And the roots were very, very close to the cortical plate. In fact, I wonder if I had CBCT in that era if I would have lifted the flap the root would have been right there; because you could feel that. So don’t forget to palpate; it’s one if the most important things. Because if you kind of feel the prominence of the root – here’s the gum over the finger; if you’re out here and you can kind of feel that prominence, you know that root’s right there.
Well now let’s come back and look at that root. In other words, Ruddle’s a big advocate of disassembly and non-surgical retreatment. That’s what I do for myself. But when we can’t be successful, then we have to have another idea; and it’s either extraction, implant or bridge.
But look at this root; let’s look carefully together. I’m reading it as coming up like this, coming around like that; I see the PDL here coming around like that. This root should have curved and gone over like that. But it was first, I imagine, blocked. What do we know? We’ve already talked about this in other shows. The block invites the what? And what happens if we keep working on the outer wall? We get a perforation.
So I believe the lingual root was blocked, ledged and perfed. But the packing is pretty remarkable. We get hydraulics; I see a portal of exit. You know, some people say these are sexy, the lateral canals. It’s not the lateral canals that are sexy; it’s the portals of exit that need to be sealed.
So this person got quite a bit of hydraulics, because I see something here. The cone ended there, and I called the other endodontist and he said he could never get to the end of the root; he was very frustrated when he packed it. And he said geez, I drove some sealer and got a little squig. So you know, that’s happened to Ruddle. And this one I don’t think I could ever kick my files back in the physiologic canal. So when I told this to the patient and the referral, we all agreed. We’ll just lift the flap and it might be two teeth. We’ll start off with the obvious one, the one that I identified was super, super sore to percussion; just light tapping, no banging with your mirror handle. So let’s go for it.
So we’ll go in there quickly. But you can see already there’s a lot of splay in these roots; I’m just showing you one angle. I could show you another angle where the buccal roots are over here, so now you know this is about a mile. Did I say a mile? I meant to say a kilometer; sorry. But the distance is quite remarkable from this root over to this root. And that’s what I’m talking about today -- challenges accessing the palatal root of maxillary first bicuspids. And I don’t have to show you a hundred. Just show you a couple and you’ll go okay, I get it. The next time I’m evaluating that tooth for surgery, or I’m going to refer it for an evaluation for surgery, I’m going to lose quite a bit of that buccal root and I’m going to make a long tunnel over there to the palatal. And I hope I have my microscope and I hope I have ideas, and I hope I can do a bloodless surgery so I can see.
So anyway, the other thing you notice is it’s up a lot higher on another plane. This one’s beveled down on this plane. This one’s beveled up here and it’s on another whole plane. So that’s how we keep root length.
Now one thing I noticed when I was doing this is I had to put quite a bit of ferric sulphate; ferric sulphate. Because I was getting a lot of bleeding. And when I was all done here, I just kind of punched through and copious amounts of bleeding. So I realized, where’s all the blood coming from? There’s no important anatomy right there. It must be granulation tissue, and granulation tissue has a profuse abundance of capillary beds; it bleeds, it’s the first tissue in disease, it’s the first tissue in wound healing. So I decided we’re here; let’s just move over. Made a separate crypt, made another hole over here, and went ahead and got the other tooth. And there we are.
So we were using the 5mm length retro instruments so we could get further up the canal, corked it nice. And you can see that if we just let a little time intervene, the bone has grown back marvelously around all the roots. You can see the PDLs coming in beautifully, and that’s endodontics.
So when we have little errors of omission, and when we have little problems sometimes because we’re not patent and we’re in a hurry and we lose our focus, sometimes we have to take those cases. Because there’s now no way we’re going to undo what we did. We can’t put the dentin back, so now we have to go think of another way. And surgery could be the approach with just – again, recognize when you start to see divergence, you start to do – whatever religion it is, you do something to help you along.
And this will be the last case. And again, it’s tied up in an extensive amount of dentistry; the costs, the stakes are high. I talked about of course, if you know Ruddle the consultation involved talking about accessing through the bridge abutment. It’s double abutted; you can’t see that, but I’ll do it like that. It’s double abutted, so it’s a 1,2,3,4-unit bridge.
But notice we have posts. They’re not long posts; they’re not threatening. This is paste, that’s not gutta-percha. Is it brick-hard paste, does it have some kind of a cortical material to keep it soft? These are things we don’t know and we can’t get the history on it.
So after weighing all that, the patient said well can you just leave everything alone? Because I have like $1200, $2400, $4800; I have about $5000 worth of dentistry invested, and that way we won’t touch it. So we said fine; we’ll go in the other way.
The lesion looks to be apically. I don’t see a component laterally; I don’t see an infrabony pocket where we could have a POE feeding that. These are all things we’ll talk about when we get more into endo/perio, perio/endo. Is it a lesion of periodontal origin, is it a lesion of endodontic origin? Those are all things we’re going to want to know.
And we’ve talked about that, right, so you already have a little clue on that. But what I can see after our discussions from today earlier, we need to do about probably 5,6,7 hours and we’ll add a show on the continuum where we’ll talk about all the things than encompass that.
So end to this case. I wanted to trace the sinus track. There was fornix of the vestibule, there was a sinus track, and we can trim off the non-useful end of the gutta-percha cone and slide it back in there and take another film. It looks like a mistle from 50 yards. I just watched the Olympics; it might be a piece of a javelin. All right. Everybody’s serious, so maybe you can smile just a little bit out there. Maybe you’ll feel just a little better if you smile. Smile; the world’s going nice.
So you cut right to the chase. Again I like these little longer preps. You’re noticing some can be 3mm, some can be 5mm. But the more space we eliminate as being a source of potential infection to the attachment apparatus, the more successful our results.
So I think we have a healing case shot in here, and there it is. So look at how our lesion appears to be kind of like this; you saw me trace it with a gutta-percha cone. And now you can see how tight the bone is. And again, properly performed endodontics is the cornerstone of restorative and reconstructive dentistry.
I hope you’ve enjoyed the approaches to the posterior roots, and I’ll leave you with one last comment. Because the lingual root, the palatal root is so far to the lingual, be sure you measure twice because you can only cut once.
CLOSE: What Does Phyllis Think? – Legacy
Okay, so when I look to my right, I see Phyllis, so it must be time for another episode of What Phyllis Thinks.
And how did you barge in here?
Okay, since this is Season 11, Road to 100, Phyllis has been thinking a lot about legacy, because this is the theme of the season. So just to reiterate, legacy is a measure of the impact you have on others; what they say, what they do, what they think as a result of having known you.
So today we’re going to ask Phyllis a question or two about what she thinks about Dad’s legacy. But then also we’re going to talk about her own legacy as a wife, mother, grandmother, and philanthropist. So are you ready for some questions?
I’m ready.
Okay, so what is the biggest priority in your life, both short term and long term?
It’s pretty much been taking care of my family; period. That’s what I do. Every day I wake up and that’s what I do.
Gosh, that’s unselfish.
I feel like you take care of me, so thank you.
You do a good job.
All right, next question. If you could say a few sentences about Dad’s legacy, what would you say?
It started accidentally because he liked to teach. And once he started teaching and doing that, one thing led to another and it created his whole journey and legacy.
So you think of Dad as a teacher; that’s the first word that comes to mind when you think of his legacy?
He started teaching in college. When he was taking all the sciences and everything, he was doing a lot of tutoring on the side and it helped him learn things better and it helped those around him. That was kind of the beginning before dentistry.
Okay. What is your role in Dad’s legacy? How have you facilitated it? I’m asking this question because I know for a fact that you have played a very large role in who he has become, and vice versa. I just want to hear it though from your perspective.
I am naturally organized, and I loved being organized. When I was three years old, I had a little filing cabinet that I was keeping notes in. I was born that way.
It’s sad.
I know. It’s a challenge that I just loved doing, and I will dive right in and take care of the details. And that is where I fit into what we’ve done together.
You know, I guess when I think of things, I think of you as the kind of person that gets things done. I also have witnessed you handle situations that were not going well, and I’m always amazed at how calm and methodical you are in solving a problem; whereas I feel like just chaos.
I’ll just interrupt. In the dental office when you say organization: champion. I mean pictures of everything that we did so when there was new people that came, they could look at tray setups and recommend or suggested speech; everything to do with patient care. She’s the one that put us on a Swiss train.
However, I do want to say that if you walk into your office, you might not be thinking organization, but it’s there.
But I know where everything is.
Well how about your own legacy? How do you hope to be remembered, in a couple sentences?
I would say number one I’m loyal and I help people. I think being remembered for that is probably the highest you can do in life is being a helper.
Okay.
Are you going to mention how you put a bunch of Indian dentists on a plane and flew them free to Amsterdam?
That’s coming. That’s how you remember Mom.
Oh, well that’s the helper.
Okay. So this September you and Dad will have been married 57 years. And your marriage for me, and for many others, is an example of how I would like my marriage to be. And I think Adam, my husband, is tired of hearing about it. But what has been the secret to your successful marriage?
Well number one, true love. The minute I met him I knew he was the one; and that has never changed. And when you build on that, if you believe it’s meant to be you’ll figure out what to do to get there.
And we had common goals pretty much along the way, and I realized early on that that was important; to be going in the same direction, the same path. I tried to branch out a couple times with my computer stuff, and he really just needed me to be with him going forward the same thing.
And a lot of it is just destiny and a sense of humor is crucial.
All right. Well I think we’re getting kind of closer to what Dad’s question was; or his comment. But you have become known as a generous donor in our community. You have donated to the kids’ schools, the Sheriff’s Association, animal places, Tennis Association, the Karate Dojo where my family trains, and I’m sure there’s more that I don’t even know about. So what motivates you to donate to these organizations?
I figure if I have it and can help somebody else, that’s a good thing. And I also like to be able to give people something that maybe I didn’t get to have. There wasn’t anybody behind me handing things out. So that’s a lot of my motivation is helping because I like to.
Okay. Next question. A large part of your generous donations to the grandkids’ schools growing up came through the annual school auction. Now people would always come up to me after the auctions and say your mom is so generous and amazing. And I would then mutter under my breath, well she’s actually quite competitive in auctions and can’t stop herself. So what did you like about the school auctions?
Well again, you had to have the money to be able to be generous.
To be the highest bidder.
To be the highest bidder. I found it – well, I guess I’m more competitive than I present. But I just found it so exciting to force people. Sometimes I’d step out at the last minute and they’d be stuck with it. It was like making them give to a good cause. I can remember when I was doing it, he’d be sitting next to me say do we have it; do we have it?
Well you got to staggering numbers, and I thought these kids need to have schoolbooks.
Oh, and it’s a write-off.
Yes, that’s her favorite word: write-off.
All right. So you are also very generous with close family as well as extended family. So is the motivation to give in these instances different?
Probably slightly because it’s family. But again, it’s helping somebody have something or go further than I was able to.
You have been very generous in the field of dentistry; helping doctors financially. Can you explain? Or maybe Dad wants to answer this one.
Well free courses. We gave a lot of free courses over the years.
You did.
Yeah, when we’d have an empty spot in our seminar or something, I had a little list of people.
From the neighborhood clinics around town. I remember you inviting dentists over.
Yes. And I would try to pick the ones that I knew would appreciate it. There are those in life that want a freebee, but I don’t feel they deserve it. Now maybe that’s judging on my part, but just experience.
And then we’ve helped a few doctors over the years attend maybe a big meeting or something that they weren’t able to come to on their own, and we’d donate to that. So I enjoy doing that.
Okay. Well, being married to Dad, you both have a public life and a private life. So do you think those closest to you will remember you a little differently than the public?
Probably so. I tend to be more even keel; kind of like the lady behind the scenes when I’m in public. But behind the scenes, I do have a lot of funny things.
Okay, she’s very mischievous. I can say that. And she also has quite a sense of humor and –
Phyllis is an enigma wrapped in a mystery.
Okay, the last question. Did you have any idea 40-50 years ago where you would be today? Did you intentionally create your future, let it evolve however, or a combination of both?
I had no idea. I dove in, I thought I was getting married to somebody who could take care of me. And that was true in a way, but it required me to work along the way myself. I always thought I would go back to college once we got him out of all of the education thing I thought I would go back to college and get a degree. But it just didn’t happen and wasn’t necessary, and I ended up with all of these careers in spite of my education or the lack thereof. I could go into bookkeeping, management, assisting, teaching; I could even -
Computer programming.
Computer programming. I could even do hair. So I ended up with a lot of occupations accidentally.
Who said “Don’t let your schooling interfere with your education”?
Absolutely.
Well when I was making these questions, I was just thinking wow! I can’t even imagine my life without Mom. Well obviously I wouldn’t be alive without Mom. But I just can’t imagine going through life without you, so you add so much to my life and my family’s life. Both of you do, so thank you very much.
Well thanks for joining the show, Kiddo.
Okay, well that’s our show for today. See you next time on The Ruddle Show.